-
PDF
- Split View
-
Views
-
Cite
Cite
Ranajit Panigrahi, Amita Kumari Mahapatra, Nishit Palo, Ashok Priyadarshi, Neglected Pipkin's fracture dislocation with bilateral femoral shaft fractures: an unusual combination, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv013, https://doi.org/10.1093/jscr/rjv013
Close - Share Icon Share
Abstract
A hip fracture dislocation with contralateral femur fracture is a rare combination. We report a case of neglected posterior dislocation of hip with Pipkins-II femoral head and medial condylar fractures associated with a contralateral femoral shaft fracture. Right hip joint was approached via the Kocher-Langenbeck, following reduction, femoral head fragments were fixed with two 4-mm cannulated cancellous screws with open reduction internal fixation plating of ipsilateral femoral condylar fracture and closed reduction internal fixation nailing of left femur in the same sitting. Immediate postoperative X-rays were satisfactory. Postoperative period was uneventful. Over 7-year follow-up, patient is successfully performing his duties with X-rays bearing no signs of avascular necrosis (AVN) or hip arthritis. Thus, complex femoral fractures require a multidisciplinary approach for successful treatment. Early congruous reduction, anatomical fixation and early rehabilitation help in reducing the incidence of AVN and postoperative arthritis. Successful diagnosis of Pipkin's fracture dislocations requires use of CT, MRI and ultrasound in adjunct to X-rays.
INTRODUCTION
A hip fracture dislocation with contralateral femur fracture is a rare combination, but the incidence is fast growing due to the increased road accidents. Femoral head fractures were first described by Birkett and fracture dislocations were first described by Pipkin [1]. These complex injuries require a prompt multidisciplinary approach and involvement of multiple specialties for successful patient management, but a universal treatment protocol is lacking due to the lack of established studies [2–4]. The majority of femoral head fractures are missed on initial presentation [2] due to unavailability of higher investigative modalities and underdiagnoses, thereby worsening the patient's condition. We report a case of neglected posterior dislocation of hip with Pipkins type II femoral head and medial condylar fracture associated with a contralateral femoral shaft fracture, an unusual combination which, to the best of our knowledge, has been seldom described.
CASE REPORT
A conscious and oriented 20-year-old male student was brought to casualty following a road traffic accident, 21 days ago where his car hit a tree besides the road, while he was sitting in the front beside the driver. Patient received primary treatment at local government hospital and was admitted there, following which patient was brought to our hospital due to dissatisfaction. On arrival, he had a Glasgow score of 15, hemodynamically stable with bilateral upper tibial skeletal traction Steinmann pins.
On examination, right lower limb was adducted, externally rotated with apparent shortening of the right lower limb, whereas the left lower limb was flexed, abducted and externally rotated. Gross swelling and bruising was present over both the upper thighs with multiple abrasions. Tenderness, crepitus and abnormal bony mobility were present at multiple levels over right thigh and middle of left thigh. Passive movements at both the hip and knee were painful and actively not possible bilaterally. Multiple abrasions were present over right leg and foot, some of which were infected. Patient had a right-sided foot drop with loss of dorsiflexion at right ankle and sensations along the dorsum of leg and foot.
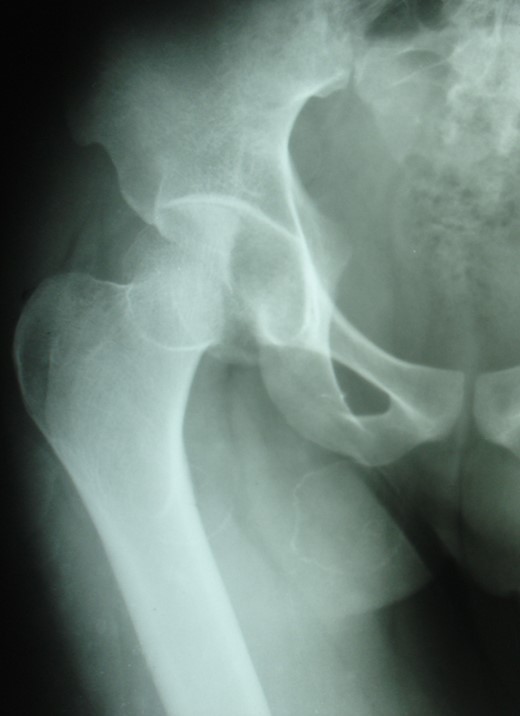
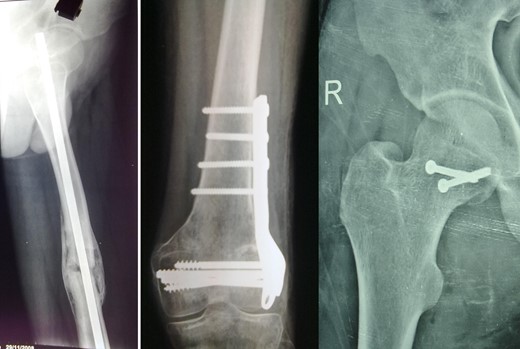
Blood parameters were within normal limits. X-ray of the pelvis revealed a right posterior hip dislocation with Pipkins's type II fracture (Rt) and ipsilateral distal medial condylar fracture with a fracture shaft of femur (Lt) (Figs 1 and 2). A CT scan confirmed the infrafoveal right-sided Pipkin's-II fracture of the femoral head (Fig. 3). A nerve conduction velocity study of lower limb suggested neuropraxia of sciatic nerve. Following attempt of closed reduction, CT scan and X-rays revealed incongruous reduction.

Initial X-ray: left thigh (anteroposterior view) and right knee (oblique view).

Initial CT scan: Pipkin's fracture (white arrow) with posterior dislocation right hip.
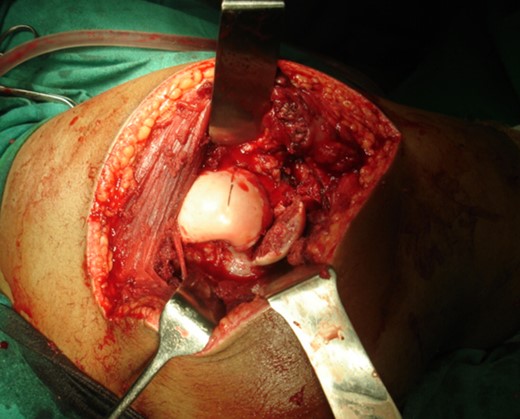
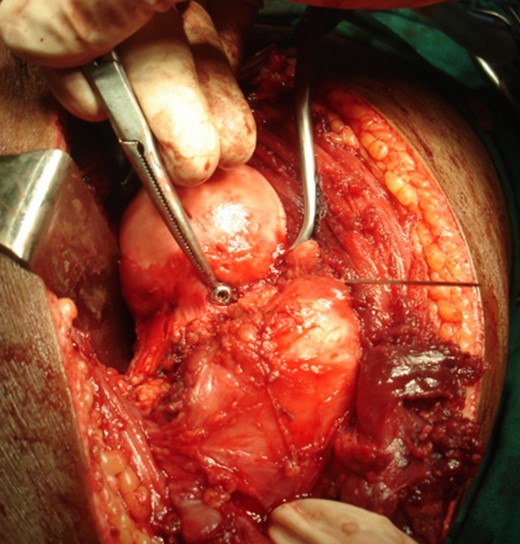
The right hip joint was approached via the Kocher-Langenbeck approach, fracture site was exposed with removal of fibrous tissue and the fracture involved mostly the infrafoveal non-weight bearing surface of the femoral head (Fig. 4). Following reduction of fracture, femoral head was fixed with two 4 mm cannulated cancellous screws that were introduced over a guide wire from the non-articular part under C-arm guidance (Fig. 5). Open reduction and plating was performed for the ipsilateral femoral condylar fracture. Closed reduction and intramedullary nailing of left femur was performed in the same sitting. The immediate postoperative X-ray was satisfactory (Fig. 6). The postoperative period was uneventful.

Patient was discharged 2 weeks following operation, then reviewed weekly for 4 weeks, monthly for 1 year and 6 monthly then after. Static quadriceps and ankle toe mobilization exercises initiated at 3 postoperative days with frequent side changing. Knee mobilization and walking were started at end of 8 weeks post-surgery. Patient's general condition was improving significantly over subsequent follow-ups. Quadriceps wasting of 1.5 cm was managed by quadriceps strengthening exercises, and gradually the tone improved.
At 1- and 7-year follow-up, X-rays were satisfactory with no signs of osteonecrosis of femoral head (Figs 7 and 8). Nail from the left femur and right distal femoral plate were removed at the end of 2 years. The patient at 7 years post-surgery had a good functional assessment (Friedman and Wyman) score with X-ray bearing no signs of avascular necrosis or heterotrophic ossification, and the fracture had united. Over 7 years, patient who is a student by profession is bearing full weight and is successfully performing his personal and social duties. The active range of motion at right hip was 0–110° flexion and 0–10° extension, external rotation 0–30° with internal rotation 0–10° with slight loss of terminal abduction (Figs 9 and 10).



DISCUSSION
Incidence of complex femoral fractures are on a rise due to increased road traffic accidents, result in extensive soft tissue injuries with bone comminution resulting in difficult patient management and fracture union problems [5]. These injuries are associated with multiple organ damage. Accurate diagnosis is essential and requires an anteroposterior view of pelvis including both hips, with oblique and lateral views of the injured hip supplemented by CT/MRI scans. Immediate reduction is key to prevent complications like avascular necrosis or heterotrophic ossification and to improve prognosis. Open reduction and fixation has become primary treatment for hip dislocations associated with femoral head fractures.
A literature suggests conservative treatment when the acetabular or femoral head fragments realign to its position and follow reduction of the dislocation and excision of the osteochondral head fragments below the fovea with larger fragments either removed or reduced and fixed using countersunk Arbeitgemeinschaft fur Osteosynthesfragen (AO group) screws, Herbert screws and bioabsorbable pins or even arthroplasty.
Treatment options for shaft fracture fixation vary from latest reconstruction nails, simultaneous transcervical screwing and shaft plating, retrograde intramedullary nailing with femoral neck-lag screws, reversed intramedullary fixation with cephalomedullary locking with their own surgical difficulties yet operative procedures are not yet standardized and a uniformly accepted treatment algorithm does not exist.
The main complications associated are avascular necrosis of the femoral head, heterotopic ossification, peripheral nerve damage and osteoarthritis. Osteonecrosis represents a most devastating complication with an incidence range of 6% at an average follow-up of 32 months [6]. Although various studies [1, 6–10] report avascular necrosis (AVN) and arthritis incidence from 8 to 25% and 12 to 20%, respectively, with Pipkin's fracture discloations, we attribute early congrous or near congrous reduction, anatomical fixation and early rehabilitation in reducing incidence of AVN and postoperative arthritis, as seen in this case. Radiotherapy and oral indomethacin have both been shown to be of benefit for prophylaxis against heterotopic ossification.
To conclude, multiple fractures of femur are difficult to treat. Initial resuscitation of patient is challenging. A multidisciplinary approach required for successful treatment. Successful diagnosis requires use of CT, MRI and ultrasound in adjunct to X-rays. Physiotherapy plays important role in recovery and rehabilitation.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- magnetic resonance imaging
- arthritis
- diagnostic radiologic examination
- roentgen rays
- ultrasonography
- fractures
- dislocations
- femoral fractures
- femur
- femoral head
- follow-up
- fracture fixation, internal
- hip joint
- osteochondritis dissecans
- diagnosis
- rehabilitation
- open reduction with internal fixation
- humeral fractures, medial condylar
- femoral fractures, condylar
- posterior hip dislocation
- femoral shaft fractures
- sitting position
- fracture dislocation of hip joint
- hip arthritis



