-
PDF
- Split View
-
Views
-
Cite
Cite
Nasra Alam, Shady Zeidan, Michael Lamparelli, A rare case of umbilical hernia containing the pancreas, Journal of Surgical Case Reports, Volume 2014, Issue 2, February 2014, rju006, https://doi.org/10.1093/jscr/rju006
Close - Share Icon Share
Abstract
We present an extremely rare case of anterior abdominal wall hernia containing multiple viscera and the pancreas in a morbidly obese patient.
CASE REPORT
A 56-year-old lady presented with a 1-day history of increasing abdominal pain, nausea and large long-standing abdominal wall hernia.
Her past medical history included morbid obesity with a body mass index (BMI) of 63, hypertension, agoraphobia, anxiety and depression. The paraumbilical hernia had been present for nearly 20 years and gradually increased in size to dominate her abdominal wall. She had very limited mobility at home and was usually cared for by her daughter.
Initial assessment revealed a massive paraumbilical hernia with necrotic patch of skin and generalized tenderness in the abdomen. She was tachycardic and tachypnoeic. Arterial blood gas analysis showed a pH of 7.46, a low PO2 and a raised lactate at 2.4. Her inflammatory markers were raised and she suffered an acute kidney injury. Urine output was poor and she was catheterized. She was primarily managed with fluid resuscitation and intravenous antibiotics.
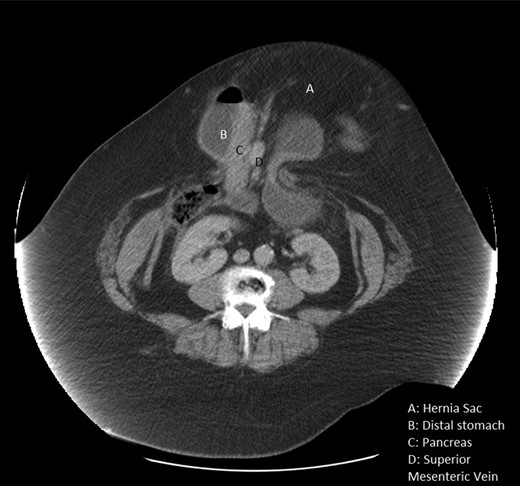
A computed tomography (CT) scan showed a large abdominal hernia containing loops of small bowel, sigmoid colon and transverse colon. In addition, the gastro-duodenal junction was in the sac pulling with it part of the posterior wall of the stomach, second part of the duodenum and the head of the pancreas (Fig. 1). The sigmoid colon had diverticular disease with evidence of perforation contained within the hernia sac.
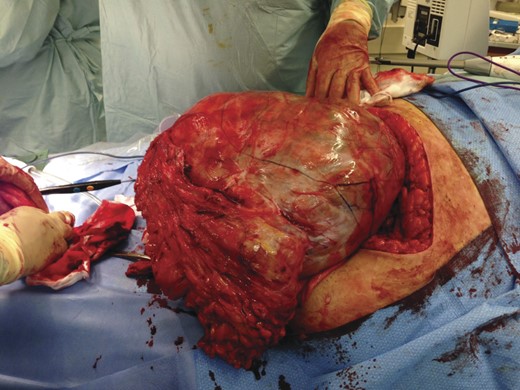
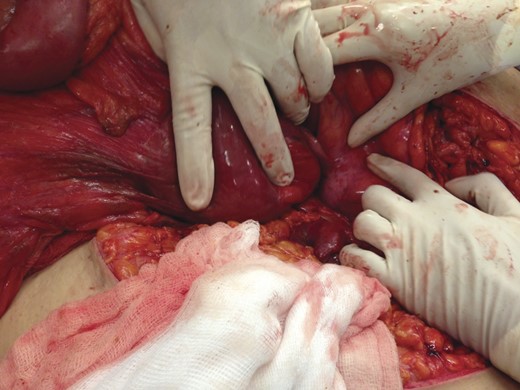
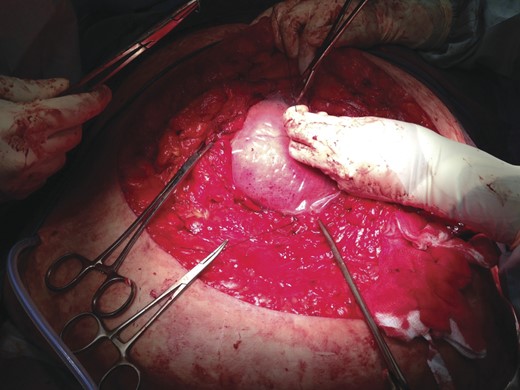
During an emergency laparotomy (Fig. 2), the hernial sac was identified and opened (Fig. 3). Contents included small bowel, large bowel, stomach and pancreas (Fig. 4). The sigmoid diverticular perforation was identified and a Hartmann's procedure was performed. The hernia contents were placed back into the abdominal cavity and a bagota bag was used (Fig. 5). The skin and fat was closed over the cavity and the patient was transferred to the intensive care unit with a view of a relook laparotomy and closure using a Permacol™ mesh within 48–72 h.

Morbidly obese patient with large umbilical hernia prepared for emergency laparotomy.
Post-operatively, she was very unstable requiring vasopressors to maintain her blood pressure and had oxygen saturations of only 85% on 100% oxygen. Her renal function continued to deteriorate and the acidaemia worsened. She developed multi-organ failure and unfortunately died 24 h later.
DISCUSSION
Umbilical and paraumbilical hernias are common in adults. They can be congenital; however, 90% are acquired defects. They are usually found in obese women, cirrhotic patients and multiparous women. Contents are usually omental fat or small bowel loops.
It is extremely rare to find the pancreas involved in any abdominal cavity hernia. There are only a few cases reported in the medical literature. In the majority of them the pancreas had herniated through the diaphragm into the thoracic cavity. Only one reported the pancreas herniating through the anterior abdominal wall [1].
Coughlin et al. [2] report a case of a type IV para-oesophageal hernia containing the entire stomach and mid-body of the pancreas. Tagaya et al. [3] discuss a patient with a para-oesophageal hiatal hernia with an incarceration of the pancreas and jejunum which was treated successfully with laparoscopic surgery. Similarly, Saxena et al. discuss surgical management of a large hiatus hernia containing the whole pancreas [4].
The only similar case that we know of [1] is from Belgium. A 65-year-old lady had a longstanding giant umbilical hernia present for over 30 years. It contained the antrum, duodenum and head of the pancreas. The incarceration of the head of the pancreas in the umbilical hernia led to an episode of acute pancreatitis [1].
Umbilical hernias and paraumbilical hernias have a higher risk of incarceration in obese patients [5]. There is evidence to suggest that patients with a BMI >60 kg/m2 had the greatest risk of incarceration [5].
We recommend that surgeons should consider surgical repair for umbilical hernias in obese patients to avoid the risk of incarceration and the higher incidence of morbidity and mortality associated with emergency operations in this group of patients.



