-
PDF
- Split View
-
Views
-
Cite
Cite
Simon M. Scheck, Rishi Ram, Benjamin Loveday, Savitha Bhagvan, Grant Beban, Crohn's disease presenting as gastric outlet obstruction, Journal of Surgical Case Reports, Volume 2014, Issue 12, 1 December 2014, rju128, https://doi.org/10.1093/jscr/rju128
Close - Share Icon Share
Abstract
We present a unique presentation of Crohn's disease in a 25-year-old male with a 3-month history of progressive gastric outlet obstruction symptoms including reflux, vomiting, postprandial pain and weight loss, with no other symptoms. Multiple imaging investigations as well as gastroscopic biopsies revealed a non-specific prepyloric lesion, without evidence of malignancy. A distal gastrectomy was performed. Subsequent histological evaluation revealed gastroduodenal Crohn's disease. Follow-up revealed no evidence of disease elsewhere in the gastrointestinal system or systemically. While it is not uncommon for Crohn's disease to involve the stomach and duodenum, it is rare for gastroduodenal disease to be the initial presentation. Isolated gastroduodenal Crohn's disease typically presents with non-specific gastritis-like symptoms over a number of years. This patient had a unique course of Crohn's disease with rapid onset of symptoms, predominantly relating to gastric outlet obstruction and no prior or subsequent history of gastrointestinal symptoms.
INTRODUCTION
In 1932, Burril Crohn first described Crohn's disease as regional ileitis [1]. The first documented case involving the stomach was published in 1949 [2]. By 1979, a further 17 cases had been reported [3]. With improvement of diagnostic modalities over time, a study in 1997 reported that 8% of Crohn's disease involved the proximal gut (mouth to jejunum) [4]; however, more recently it has been suggested that 30–50% of patients with Crohn's disease have proximal involvement [5]. Despite increasingly apparent proximal gut involvement, only 0.5–4% of Crohn's disease involves the stomach and/or duodenum [6]. Among patients with gastroduodenal involvement, ileocolic disease is typically apparent at the time of gastroduodenal symptoms [6]. Here, we describe a case of isolated rapidly progressive gastroduodenal Crohn's disease.
CASE REPORT
A 25-year-old male was referred to our surgical department for investigation of 3 months of progressive gastric outlet obstruction. At presentation, the patient was unable to tolerate oral intake other than minimal amounts of water. There was a 13-kg weight loss over this 3-month period (weight 79 kg at presentation).
Gastroenterology work up was undertaken shortly after the onset of symptoms. Endoscopy at that time showed non-specific duodenitis, with biopsies taken from the gastric antrum and body as well as the duodenum. Gastric mucosa showed a mild-to-moderate increase in chronic inflammatory cells in the lamina propria with few focal polymorphs. Helicobacter pylori were present. No epithelial dysplasia or malignancy was reported. Duodenal biopsy showed no evidence of increased lymphocytes, parasites, dysplasia or malignancy. Triple therapy was initiated to eradicate H. pylori. CT did not reveal any abnormality of the gastrointestinal tract. Symptoms improved with eradication therapy. While subsequently on holiday in Taiwan the symptoms returned, prompting further investigation. Endoscopy identified a possible submucosal lesion in the duodenum. Endoscopic ultrasound suggested a duodenal lesion (suboptimal study). Inflammatory markers were raised at this point. As the patient remained unwell, he returned to New Zealand for further evaluation in our centre.
The patient was a previously well non-smoker, with no significant medical or surgical history, taking only omeprazole (prescribed during the prior work up). There was a family history of Crohn's disease in a maternal aunt.
On admission, the patient was haemodynamically normal, oliguric and afebrile with mild peripheral oedema. Abdominal examination revealed a soft, non-tender abdomen with no masses.
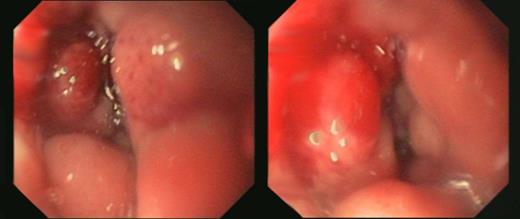
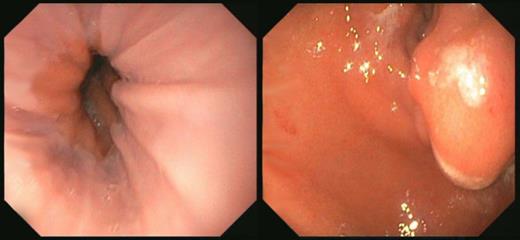
Endoscopic images of the lower oesophagus (left) and prepyloric stenosis (right).
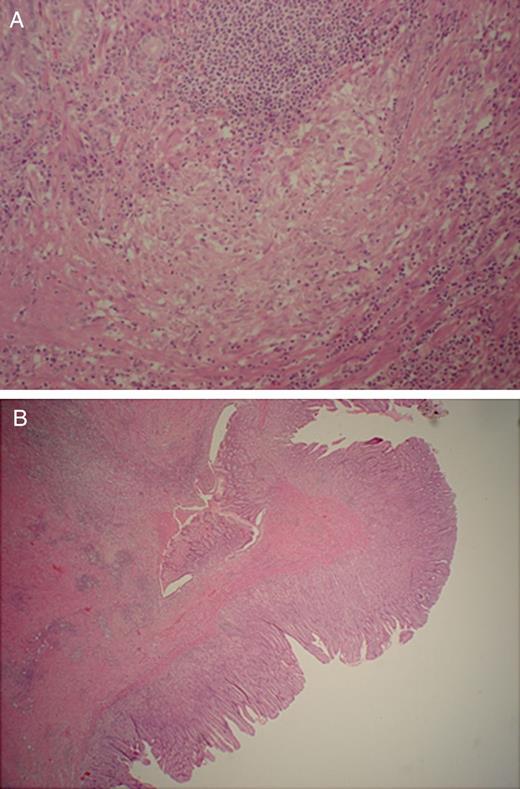
(A) Epithelioid granuloma away from sites of ulceration (×20 H&E). (B) Antral stomach with fissuring ulceration with Crohn's-like lymphoid aggregate formation (×10 H&E).
The patient was discharged 14 days after the operation when he was able to tolerate adequate oral intake for nutritional need. Subsequent anti-saccharomyces cerevisiae antibodies testing was positive for both IgG (66 units/ml) and IgA (171 units/ml). The patient was subsequently started on azathioprine. Colonoscopy and gastroduodenoscopy with multiple biopsies have failed to show any evidence of further disease.
DISCUSSION
Isolated gastroduodenal Crohn's disease represents a known diagnostic dilemma, with biopsies often showing non-specific inflammation [7]. Where tissue diagnosis is not conclusive, diagnosis should be considered based on symptoms, endoscopy, multiple biopsies and radiological findings [5].
In the case reported here, the diagnosis was not apparent until histological analysis of the distal gastrectomy specimen was undertaken, despite multiple imaging modalities including CT and both external and endoscopic ultrasound, as well as histological analysis of multiple biopsies directly from the affected regions. There was no evidence of more distal disease. This is not unique among upper gastrointestinal Crohn's disease cases; however, this case is unlike other cases to our knowledge due to the rapid onset of symptoms of gastric outlet obstruction with no long history of gastritis-like symptoms. Documented cases of isolated upper gastrointestinal Crohn's disease typically present with gastritis-like epigastric pain progressing over a number of years [7–9]. Symptoms of gastric outlet obstruction (bloating, vomiting, postprandial pain and weight loss) evolve in many cases, but almost universally after years of gastritis-like symptoms. Importantly, the case we present here did not have any previous history of gastritis-like symptoms, and had rapid onset of symptoms of gastric outlet obstruction with a 3-month progression from tolerating normal diet to tolerating only small sips of fluid. We are aware of one other similar case in which a 42-year-old woman presented with a 9-month history of progressive epigastric pain, nausea, vomiting, weight loss and eventually food intolerance [10]. Despite multiple investigations including radiological and endoscopic imaging, a diagnosis was not able to be confirmed prior to the need for surgical intervention to relieve gastric outlet obstruction. Histological diagnosis confirmed Crohn's disease post-operatively (the distal ileum was also found to be affected). The similarities between the present case and this case from 1977 emphasize the difficulty in diagnosing atypical Crohn's disease, despite advances in medicine over the past 30 years.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
We acknowledge and thank the patient for allowing publication of this report. We also acknowledge the efforts of pathologist Dr Jane Evans for the histopathological images, and gastroenterologist Dr Tim King for endoscopic images.



