-
PDF
- Split View
-
Views
-
Cite
Cite
Oliver McLaren, Spontaneous idiopathic recurrent pneumoperitoneum, Journal of Surgical Case Reports, Volume 2013, Issue 8, August 2013, rjt071, https://doi.org/10.1093/jscr/rjt071
Close - Share Icon Share
Abstract
Pneumoperitoneum, gas under the diaphragm, is often a sign of significant intra-abdominal pathology, be it perforation in the stomach or duodenum secondary to peptic ulcer disease or in the small or large bowel as a result of inflammatory bowel diseases, diverticulitis or cancer, it can also be iatrogenic as a result of endoscopy or laparoscopy. The diagnosis is made with erect chest and abdominal radiographs, air is usually most visible under the right hemi-diaphragm. Here, we present a troublesome case of recurrent pneumoperitoneum, which despite extensive investigations and laparotomy no cause was found.
INTRODUCTION
Pneumoperitoneum is a radiological finding most commonly associated with significant intra-abdominal pathology. In over 90% of cases, pneumoperitoneum is the result of perforation of a hollow vicus [1]. Rarer than this is ‘spontaneous pneumoperitoneum’ with intra-thoracic, gynaecological or iatrogenic aetiology. In even rarer cases, intra-abdominal, intra-thoracic, gynaecological and iatrogenic causes have been ruled out, and we are left with spontaneous idiopathic pneumoperitoneum, which in this case was a recurrent phenomenon.
CASE REPORT
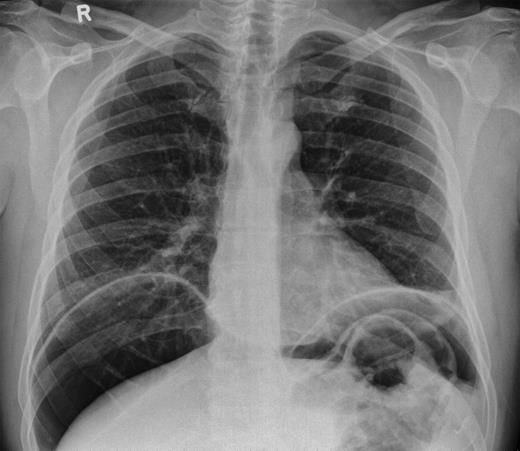
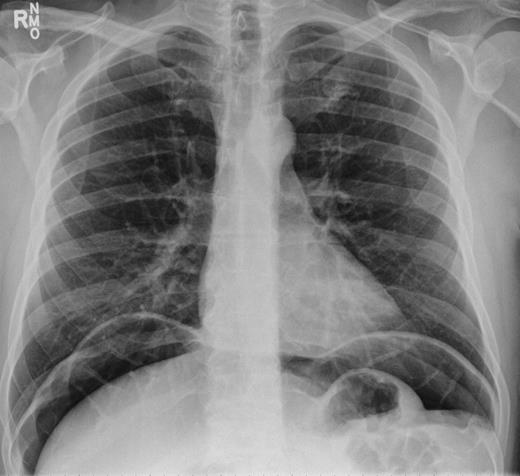
In 2011, a 46-year-old man presented with an acute abdomen. Patient had a 3 day history of abdominal pain with dyspepsia, initially epigastric with pain radiating to his shoulder. He had no associated symptoms of nausea, vomiting or change in bowel habit. There was no history of peptic ulcer disease, inflammatory bowel disease, diverticular disease or malignancy. His pain was refractory to standard analgesics and exacerbated by movement and palpation of the abdomen. There was no past medical or family history of note, and the patient had never experienced these symptoms before. Routine observations were normal, except for tachycardia. On examination, there were no peripheral stigmata of inflammatory bowel disease, abdomen was diffusely tender and tympanic, but soft with normal bowel sounds. Blood tests showed no significant abnormalities, and C-reactive protein (CRP) levels were not measured. Plain abdominal and erect chest radiographs showed pneumoperitoneum (Fig. 1) with Rigler's sign present around small bowel loops lower in the abdomen (Fig. 2).

He was taken for urgent laparotomy to evacuate the free gas and aid diagnosis. The bowel was extensively examined and no evidence of perforation was found. The abdominal wall was closed and he returned to the ward. Subsequent X-rays showed that the pneumoperitoneum had resolved. Post-operatively his CRP level was 226 and he went into ileus requiring nasogastric tube placement (Fig. 3). With recurrence of normal bowel activity and with settling of his symptoms, he was discharged.

Over a year later, the same gentlemen presented to the surgical admissions unit once again with a history of acute abdominal pain. The duration and nature of symptoms were very similar to his previous admission. He again underwent plain film abdomen and erect chest radiographs that showed a large volume of free air under the diaphragm (Figs. 4 and 5).

The patient was apyrexial and cardiovascularly stable, other than his acute abdominal pain, he was healthy. We managed his pain with analgesia, stepping up as required. A water soluble contrast study was arranged, this demonstrated no leak or diverticular in the oesophagus, stomach or duodenum.
He underwent a computed tomography (CT) scan of his chest/abdomen and pelvis, and this showed some upper abdominal fluid, some small sigmoid diverticulae but nil else. The scan was discussed at a regional radiology meeting to look for any diaphragmatic defects or any other cause of pneumoperitoneum, but none were found.
This man demonstrated clear pneumoperitoneum, he was extensively investigated; all blood tests were normal except for a raised postoperative CRP, his laparotomy showed no evidence of perforation, the contrast study showed no leak and a CT scan showed mild sigmoid diverticulae only. In light of all this, we reached a diagnosis of ‘Recurrent spontaneous idiopathic pneumoperitoneum’.
DISCUSSION
Spontaneous pneumoperitoneum has many causes, not all of them are surgical. It can originate from intra-abdominal and intra-thoracic causes, as well as gynaecological and iatrogenic causes. Williams et al. in 1997 reviewed causes of pneumoperitoneum.
Intra-thoracic causes include trauma, pneumothorax and others, and these can be associated with pneumomediastinum or pneumocardium. There is also an association with mechanical ventilation in intensive therapy unit patients following cardiopulmonary resuscitation [2].
Air can be found in the abdomen via the vagina, uterus and salpinx. Pneumoperitoneum via a gynaecological route has been reported following coitus and Jacuzzi usage, as well as vaginal douching [3].
Air can be iatrogenically introduced to the peritoneum via endoscopic procedures such as oesophageal-gastro-duodenoscopy and colonoscopy [4].
Intra-abdominal causes of pneumoperitoneum are better recognized as they are more common. Most of these causes are surgical in nature, and it is reported that over 90% of cases of pneumoperitoneum is the result of perforation of an intra-abdominal viscus. It is commonplace for rapid surgical intervention/exploration, not only to find the offending perforation, but to limit the degree of intra-abdominal contamination.
This was a complicated presentation of pneumoperitoneum. It presented a challenge in diagnosis and management, not once but twice. From this case, we can take an important learning point. Though the presentation of pneumoperitoneum is often suggestive of significant surgical pathology, there are instances when it can be managed conservatively and thereby avoiding the risks of undergoing a laparotomy. Despite its startling clinical presentation and radiographic findings, in the absence of cardiovascular instability it is possible to monitor these patients closely and in the right circumstances manage them conservatively.



