-
PDF
- Split View
-
Views
-
Cite
Cite
D. Hammond, N. Grew, Z. Khan, The white-eyed blowout fracture in the child: beware of distractions, Journal of Surgical Case Reports, Volume 2013, Issue 7, July 2013, rjt054, https://doi.org/10.1093/jscr/rjt054
Close - Share Icon Share
Abstract
Inferior ‘trapdoor’ orbital floor fractures with muscle and soft tissue incarceration are the most common type of orbital fracture in children. Delays to treatment can lead to a significant morbidity. It has been recommended that children who present with a ‘white-eyed blowout’ fracture should have surgery performed within 48h of diagnosis, otherwise prognosis is poor. A 14-year-old boy was initially misdiagnosed with a head injury due to the minor appearance of his orbital injury and his presenting complaint of nausea and vomiting. This resulted in a significant delay to surgery. The oculovagal reflex associated with orbital injuries is well documented (Wei and Durairaj in Pediatric orbital floor fractures. J AAPOS 2011;15:173–80). It should be considered by emergency department and paediatric staff when dealing with patients who have sustained a blow to the orbital region, despite not having a subconjunctival haemorrhage. The importance of examination to detect other features of orbital blow-out and entrapment are stressed.
INTRODUCTION
The fractured orbital floor is a common injury in adults, and is frequently caused by interpersonal violence. It is not frequently a medical emergency. However in children, it requires prompt surgical intervention, otherwise catastrophic morbidity can occur.
CASE REPORT
A 14-year-old boy was playing soccer, when he sustained a blow from a knee to his left orbit. He sustained no loss of consciousness. He presented to his nearest emergency department. He was assessed and, as he was nauseous and vomited once, a decision was made to admit him under the paediatric services to monitor his head injury.
He had minimal periorbital bruising, and his visual acuity was 6/6; however, his ability to move his eye was reduced over the next 24h, and his diplopia worsened. His nausea and vomiting continued, and he had a head CT scan performed. This showed no brain injury; however, the scan discovered a left orbital floor fracture with entrapment of the inferior rectus muscle (Fig. 1).
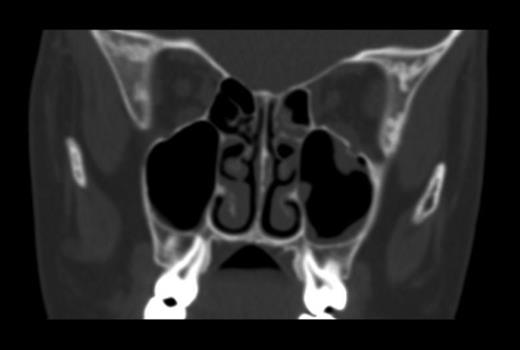
Preoperative CT scan showing a fracture of the left orbital floor with entrapment of the inferior rectus muscle.
He was subsequently transferred to our unit, and when he arrived 60h after his initial injury, his left eye showed no vertical movement and very limited downward gaze and some preserved lateral and medial movement. Movements were painful. There was no subconjunctival haemorrhage; 6/6 visual acuity; his pupils were equal and reactive to light and he had marked diplopia in upward gaze. The patient kept the eye habitually closed to avoid diplopia.
He was urgently taken to theatre, where an open exploration of his left orbit was performed. This was performed via a second crease incision, and his Inferior rectus was successfully released.
At 1 month following surgery, his diplopia and range of ocular movement has improved significantly but has not completely returned to normal. He continues to be monitored under review.
DISCUSSION
Orbital floor fractures have the potential to cause significant morbidity both in the short and long term, and commonly present to the emergency department for initial assessment. The pathway for the majority of these injuries in adult patients involves rarely involves an indication for early surgery in cases uncomplicated by sight threatening complications. Patients are often seen for a clinic review and, if necessary, later semi-urgent/elective surgery.
There is a specific subset of orbital injuries which present as an emergency clinically suggestive of a head injury. This subset, ‘white-eyed blowout’, usually occurs in patients under 18 years of age. There is a history of trauma and little sign of soft tissue injury.
Nausea and vomiting in children who have minimal signs of trauma and no loss of consciousness has been found to be a presenting sign of orbital fracture in up to 55.6% of cases [1]. A high proportion of these patients also present with bradycardia [2].
The oculovagal reflex is well described in ophthalmic surgery, but may be caused by any manner of pressure on the globe. Children with orbital blowout fractures present in a different manner from adults. The classic presentation in children is a white eye injury (i.e. no subconjunctival haemorrhage) with upgaze diplopia and general malaise [3].
CT imaging normally reveals a trap door orbital floor fracture with herniation and acute entrapment of orbital muscle and is regarded as a maxillofacial emergency. It is the fact that the injury presents with marked nausea, vomiting, headache and irritability suggestive of a head injury that commonly distracts from the true aetiology. It requires prompt diagnosis and treatment to avoid permanent morbidity.
One-third of children with orbital blowout fractures are admitted for head injury observations, while the true cause for the symptoms goes unrecognized and uninvestigated [3].
Orbital blowout fractures in children require more swift intervention than in adults if muscle ischaemia and permanent impairment of the vision is to be avoided. The delay for head injury observation may therefore compromise the surgical outcome. It is recommended that surgery be considered within 48 h of diagnosis [1].
Inferior trapdoor fractures with muscle and soft tissue incarceration are the most common type of orbital fracture in children (27.8–93%) [1]. The oculovagal reflex must be considered as a cause of nausea and vomiting.
If delays to treatment and the associated morbidity are to be avoided, then the paediatric clinician must have a low threshold for investigating a suspected orbital fracture whilst remaining vigilant for significant head injury.
REFERENCES
- craniocerebral trauma
- child
- emergency service, hospital
- orbital fractures
- pediatrics
- surgical procedures, operative
- diagnosis
- morbidity
- reflex
- subconjunctival hemorrhage
- orbital trauma
- nausea and vomiting
- fractures, blow-out
- orbital blow-out fractures
- entrapment (morphologic abnormality)
- chief complaint
- soft tissue



