-
PDF
- Split View
-
Views
-
Cite
Cite
P Narh-Martey, A Bello, D Orr, I Galdyn, Laparoscopic management of small bowel obstruction with associated intestinal ischemia, Journal of Surgical Case Reports, Volume 2012, Issue 8, August 2012, Page 4, https://doi.org/10.1093/jscr/2012.8.4
Close - Share Icon Share
Abstract
Obstruction is the most common surgical disorder of the small bowel. Complete small bowel obstruction (SBO) is usually treated surgically because bowel strangulation cannot be excluded with certainty. Acute SBO has been previously considered a relative contraindication for laparoscopic management especially due to the laparotomy conversion rate. We present a case of SBO for which laparoscopic management resulted in earlier return of bowel function, shorter hospital stay, faster overall recovery, and decreased morbidity when compared to laparotomy.
INTRODUCTION
Obstruction is the most common surgical disorder of the small bowel. Complete small bowel obstruction (SBO) is usually treated surgically because bowel strangulation cannot be excluded with certainty. This is particularly important because strangulation is associated with increased patient morbidity and mortality. Laparoscopy has been proposed as an effective management although the conversion rate to open surgery from the laparoscopic approach can often be quite high. Common reasons for conversion include inadequate visualization due to distended small bowel, iatrogenic perforations, gangrenous small bowel, and the inability to adequately relieve obstruction laparoscopically. We report a case of SBO with dense adhesions and intestinal infarction successfully treated with laparoscopy.
CASE REPORT
A 40-year-old female presented at midnight to the emergency room complaining of severe abdominal pain. She admitted to a 2-day history of abdominal pain which was constant and non-radiating. Throughout the duration of the pain, she was nauseated and vomited twice. Her last bowel movement was the day before and she denied dysuria. The patient was a relatively healthy individual prior to this presentation. Her past medical history was significant for Polycystic Ovarian Syndrome and her previous surgeries included a cesarean section performed in 1995 and a total abdominal hysterectomy two years later through the previous pfannenstiel incision. On examination, she was in moderate distress and her vitals were within normal limits. Abdominal examination revealed mild distention and generalised moderate tenderness in the lower abdomen without guarding. Laboratory data was within normal limits with a WBC count of 7.
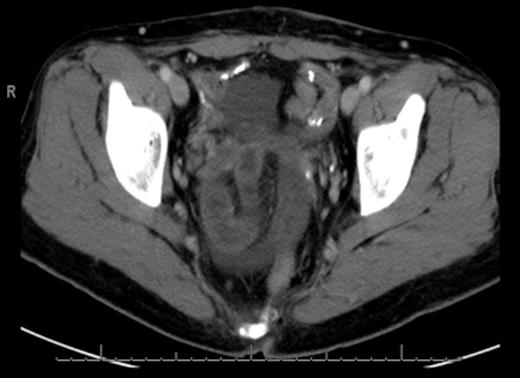
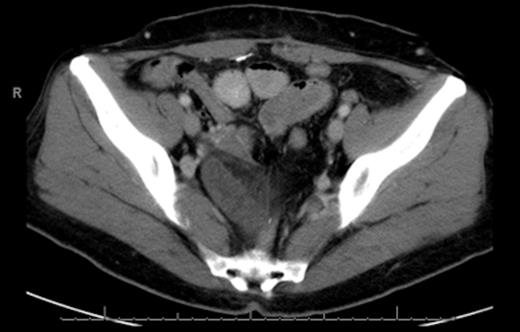
CT scan of the abdomen and pelvis revealed wall thickening and dilation of a few loops of small bowel located in the pelvis. We were not able to exclude closed loop obstruction (Fig. 1 & 2).
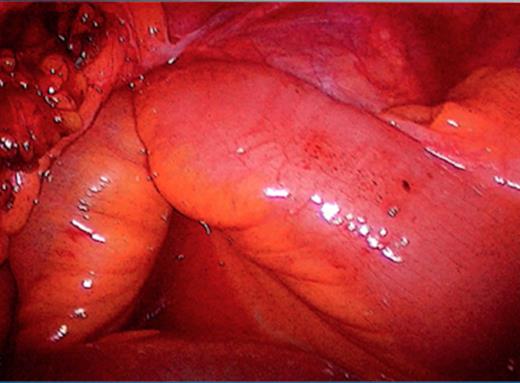
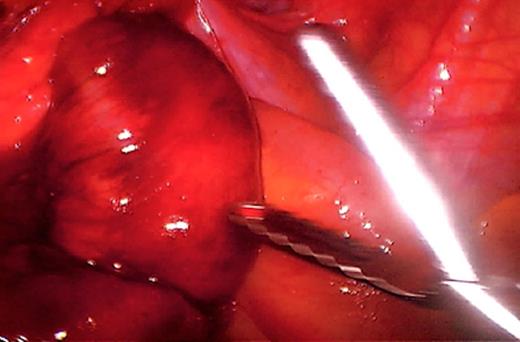
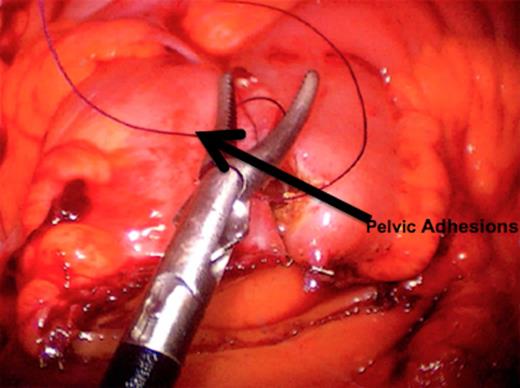
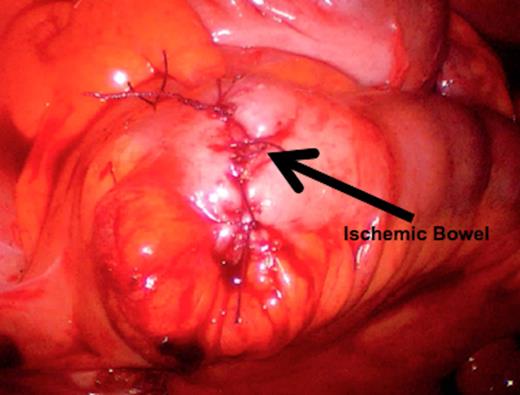
The initial management consisted of a NG tube insertion, IV hydration, and serial abdominal exams. Later, the patient was taken to the operating room due to the significant worsening of her pain. The abdomen was insufflated via the umbilicus with a Veress needle and a 5mm port was placed. Extensive adhesions were visualized throughout the pelvis which was carefully divided. The majority of the small bowel was normal in appearance (Fig. 3), but a segment of 1.5 feet was ischemic and surrounded by dense adhesions (Fig. 4).
This segment was resected and a side-to-side anastomosis was performed (Fig. 5 & 6). On POD 1 bowel function returned and she was started on a clear liquid diet. On POD 2 the patient was started on a regular diet and was discharged home the following morning. On POD 8 she was seen in the office and by then had returned to her baseline level of functioning.
DISCUSSION
Acute SBO has been previously considered a relative contraindication for laparoscopic management especially due to the laparotomy conversion rate (1). A retrospective study comparing laparoscopic vs. open surgery showed a conversion rate of 32%. In a large systematic review of 1061 cases of SBO, 705 were treated laparoscopically while the conversion rate was 33.5%.(2) Most common causes for conversion were dense adhesions (27.7%), ischemic bowel (23.1%), unidentified etiology, iatrogenic injury, malignancy, inadequate visualization, hernia and other causes (1,2). Morbidity was 15.5% and mortality 1.5% following conversion. Studies have recommended that if a conversion to an open lysis of adhesions is necessary, it should be done sooner rather than later to reduce post-operative morbidity (3).
Some surgeons recommend performing a mini-laparotomy near the site of occlusion when detected via the laparoscopic approach. This will shorten the hospital stay and decrease the conversion rate. However, in the case of our patient, her outcome was quite good despite not following this recommendation and simply removing the ischemic bowel section laparoscopically. (4) Given the relatively high rate of conversion, it would be beneficial to establish proper guidelines for conversion in the future, particularly as the laparoscopic approach becomes more of a mainstay of SBO treatment.
Several studies have described laparoscopic surgical management of SBO as safe and effective. (5-7) Many surgeons consider the laparoscopic approach to be safer than an open lysis of adhesions. (8) Surgery which lasts less than 120 minutes is known to be associated with lower postoperative mortality, making the laparoscopic approach more desirable for both the surgeon and the patient (7). This approach results in earlier return of bowel function, shorter hospital stay, faster overall recovery, and decreased morbidity when compared to laparotomy (5,9). However, these findings have not yet been confirmed in a randomized trial (9).
Many surgical interventions are now performed laparoscopically. As surgeons’ levels of confidence with laparoscopy continue to build and as safer and more cost-effective techniques are introduced, some of the reasons for conversion to laparotomy as listed above will likely be reduced or perhaps eliminated altogether. This in turn will decrease morbidity in our patients and increase the acceptance of laparoscopic management for SBO. Clinical trials may be needed to prove a clear benefit with laparoscopic management of SBO as opposed to conventional open surgery.



