-
PDF
- Split View
-
Views
-
Cite
Cite
R Van Der Rijt, P Moradi, Dermatofibrosarcoma protuberans: A rare cutaneous tumour, Journal of Surgical Case Reports, Volume 2012, Issue 7, July 2012, Page 8, https://doi.org/10.1093/jscr/2012.7.8
Close - Share Icon Share
Abstract
Dermatofibrosarcoma protuberans (DFSP) is an uncommon, locally aggressive, soft tissue tumour. Occurrence in the head and neck region is rare and facial presentations are even rarer. We present a case of a DFSP in a young gentleman with the oncological, functional and aesthetic challenges that arose from the case. We also reviewed the relevant literature on DFSP pertaining to the head and neck region and devised a treatment algorithm based on the best available evidence.
INTRODUCTION
DFSP is an uncommon soft tissue tumour, which has a high rate of recurrence despite apparently adequate surgical treatment. DFSP rarely metastasises. It’s initial appearance is usually seemingly benign.
CASE REPORT
A previously well 44 year old male presented with a 6 month history of a soft slow growing lump on his right cheek. The lump was painless and there were no overlying skin changes. His chief complaint was cutting the overlying skin whilst shaving.
He preseneted to his GP who made a provisional diagnosis of a sebaceous cyst and he was referred to a local plastic surgeon for excisional biopsy of the lump. The treating plastic surgeon excised the obvious soft tissue tumour with the resultant scar as shown in figure1.

Histopathology returned as DFSP with involved margins. He was then referred to a multidisciplinary head and neck clinic at a tertiary hospital for definitive management.
He underwent a staged elective re- excision of the residual tumour and nasolabial scar with a 2cm margin, with the deep plane being the muscular elevators of the upper lip. With a view of reconstructing the defect a week after the excision once formal histopathology was available.
Pathology demonstrated residual DFSP surrounding a recent surgical scar. Bands of tumour extended deep into the subcutis surrounding adipose tissue and infiltrating skeletal muscle. The tumour extended to the deep resection margin over a broad front.

Patient underwent a full thickness re-excisionof residual right cheek DFSP
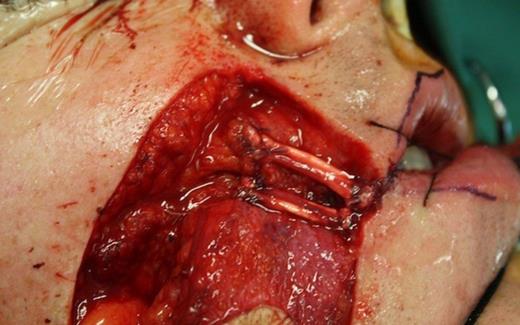
The patient then underwent a full thickness re-excision of residual right cheek DFSP including buccal mucosa, insertion of the upper lip elevators, right oral commissure and 20% of the upper and lower lips. (Fig. 2)
Prior to the resection of the tumour, the Levator Labii Superioris and the Zygomaticus Major muscles were identified and 4.0 Ti-CronTM (Covidien) modified Kessler sutures were used to secure the muscles to prevent retraction of the muscles superiorly after resection. Pathology demonstrated a focus of residual tumour 5.5mm clear of the deep margin and clear peripheral margins. The defect was templated and a left radial forearm free flap was raised with two skin paddles, one for external coverage and one for an internal lining.
Two strips of palmaris longus tendon were used to re-suspend LAO and zygomaticus major
Two strips of the left Palmaris longus tendon were used to re-suspend LAO and Zygomaticus major with 4.0 Ti-CronTM (Covidien) (Fig. 3). The flap pedicle was tunneled subcutaneously anterior to the mandible. The mucosal surface was inset prior to the microsurgical anastomosis to the right facial artery and common facial vein.

The patient had an uneventful post operative course. There has been no recurrence at 6 month follow up. Figures 4 and 5 show post operative results at 3 months.

DISCUSSION
Dermatofibrosarcoma protuberans (DFSP) is an uncommon, fibrohistiocytic tumour known to be locally invasive and with very low incidence of distant metastasis (1). Local recurrence rate is between 32% and 76% (2). However, metastatic disease is rare; it has been reported in only 4% of cases.
The occurrence of this tumour is most prevalent in the age group 20 -40 (3). A slight male predominance is suggested. The most frequently affected region is the trunk, followed by the upper and lower extremities (1-3). Head and neck cases account for approximately 10 -15% of cases (4). The occurrence of this tumour on the face is extremely rare.
Initially the tumor can be similar to a keloid, an asymptomatic indurated plaque or nodule. If left untreated it will become firm, raised, and ulcerated (5). This ambiguous, and seemingly benign clinical presentation necessitates making a final diagnosis based on extensive histological analysis.
The true cellular origin of this dermal tumour is yet to be determined. Evidence suggests that its origins may be fibroblastic, neuroectodermal, histiocytic, or a combination of the three due to mutations in multipotent cutaneous mesenchymal stem cells. Among others, immunohistochemical staining demonstrates strong positivity for CD34, which is primarily used to distinguish it from other cancers. Approximately 10% of DFSP are a more aggressive subtype with fibrosarcomatous progression FS- DFSP. FS – DFSP is associated with increased risk of metastasis (6).
In addition to physical examination, Magnetic resonance imaging (MRI) or CT may be useful in evaluating extent of tumour spread. Imaging is, however, not usually required, as DFSP is usually limited to local disease.
DFSP tumours are characterised by unpredictable and widespread subclinical extension, hence high rates of recurrence. The goal remains complete excision of tumor cells with maximum preservation of normal tissue to maintain function and an acceptable aesthetic appearance. The need for clear margins on the face creating potentially large tissue defects poses many reconstructive challenges.
Moh’s Micrographic Surgery (MMS) or staged wide excision “Slow Moh’s “(with formal histopathological sectioning and delayed reconstruction for complete circumferential peripheral and deep margin assessment) is becoming the standard surgical treatment for DFSP (7). Early literature recommends surgical margins of 4 to 6 cm, the current recommendations of surgical margins is at least 2 cm, preferably 3cm (8).
Recurrence is more common in the head and neck region, ranging from 50 -75% (9). Local recurrence typically is seen within the first 3 years after excision, where it is estimated that 80% of recurrences are thought to recur (7). Careful, regular follow up examinations for tumour recurrence are paramount.
In cases where surgery is not a viable option, or where recurrence has occurred despite multiple wide local resections, several treatment options are available.
Detectable chromosomal abnormalities in DFSP lead to an over expression of the Platelet Derived Growth Factor Ligand (PDGF). Targeted molecular therapy aims at arresting tumour growth by blocking PDGF activity. Imatinib mesylate is a potent and selective tyrosine kinase inhibitor, with efficacy against the PDGF receptors (7). It has also been reported to induce complete or partial remissions in patients with advanced or recurrent DFSP. It is most commonly used for cases of DFSP that are unresectable, recurrent or metastatic. Although not used commonly, there is growing evidence to suggest that the neoadjuvant use of targeted molecular therapy may be beneficial (7).
DFSP has been responsive to radiotherapy at doses ranging from 45-60 Gy (10). It has proven benefit as postoperative adjuvant radiation therapy in incompletely excised tumours. Its use is controversial, however, as few authors have speculated an association between the use of radiation therapy and high grade transformation. Close monitoring is required if radiation therapy is undertaken.
Chemotherapy has no proven benefit in locally aggressive DFSP and it’s efficacy in metastatic disease is undefined.
DFSP is a rare head and neck tumour arising from the dermis with a high propensity to recur. It poses diagnostic and reconstructive challenges. Based on the best available evidence we recommend a staged excision and reconstruction with at least 2cm surgical margins, preferably 3cm. If the patient is not a surgical candidate we recommend consideration of targeted molecular therapy and radiation therapy.



