-
PDF
- Split View
-
Views
-
Cite
Cite
JA Greene, PJ DiPasco, VP Koshenkov, AS Livingstone, Portal hypertension from nodular regenerative hyperplasia of the liver treated with distal splenorenal shunt, Journal of Surgical Case Reports, Volume 2012, Issue 7, July 2012, Page 2, https://doi.org/10.1093/jscr/2012.7.2
Close - Share Icon Share
ABSTRACT
Portal hypertension (PH) is a devastating sequelae of several pathologic entities, with alcoholic cirrhosis being the most common cause in the western world and endemic schistosomiasis worldwide. A much less common aetiology of non-cirrhotic PH is nodular regenerative hyperplasia (NRH) of the liver. The hallmark of NRH is a benign remodeling of the hepatic parenchyma into regenerative nodules in the absence of fibrosis (1). A Warren-Zeppa Distal Splenorenal Shunt (DSRS) was performed in a young patient with NRH of the liver to alleviate PH. This procedure was chosen due to its low postoperative rates of hepatic insufficiency and high durability.
INTRODUCTION
The Distal Splenorenal Shunt (DSRS) procedure was developed and refined at the University of Miami by W. Dean Warren and Robert Zeppa in 1967 for the treatment of PH, predominantly due to alcoholic cirrhosis (2,3). This operation was commonplace until the 1980s when advancements in endovascular stenting resulted in the DSRS being gradually supplanted by the Transjugular Intrahepatic Portosystemic Shunt (TIPS) procedure. We describe a case of pre-sinusoidal PH whose treatment with DSRS rather than TIPS reduced the long term complication of shunt thrombosis associated with TIPS, and maintained hepatopetal nutritional blood flow to the liver. NRH of the liver was proven to be the aetiology after biopsy.
CASE REPORT
A 41 year old man with a 20 year history of Crohn’s disease was referred because of enlarging, massive abdominal wall varices, splenomegaly with thrombocytopenia, but no ascites (Fig. 1). History was notable only for Crohn’s disease and laparoscopic inguinal hernia repair in 2004. The gastroenterologist managing the patient’s Crohn’s disease noted the patient’s abdominal wall varices and a thorough workup ensued. Endoscopy revealed Grade 2 esophageal varices. Alpha-1 antitrypsin, serum ceruloplasmin, ANA, and antimitochondrial antibody studies were all negative. Liver biopsy revealed no cirrhosis with minimal portal inflammation, no significant fibrosis and no evidence of malignancy. A bone marrow biopsy revealed no evidence of malignancy or ITP.

The portal venous phase of superior mesenteric vein (SMV) angiography demonstrated hepatopetal flow into the liver, no arteriovenous communication, and a large umbilical vein decompressing the portal system. Free and wedge hepatic vein pressure measurements were normal. Direct catheterization of an abdominal wall varyx measured 26 mmHg pressure, confirming the severity of the portal hypertensive state. With enlarging esophageal and abdominal wall varices and confirmation of severe pre-sinusoidal PH, the patient was offered a DSRS as an effective and durable solution. Preoperative confirmatory hepatic catheterization and angiography performed two days prior to surgery confirmed the hepatic wedge pressure and provided accurate portal venous anatomy.
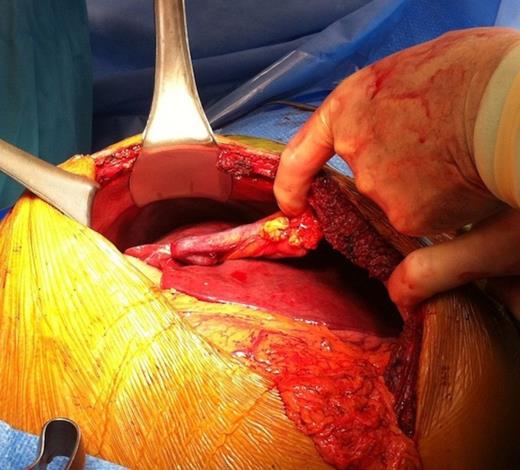
The abdomen was explored via a generous subcostal incision extending from the left anterior axillary line to the right midclavicular line. Engorged paraumbilical veins and abdominal wall varices were encountered and ligated to preserve hepatopetal flow (Fig. 2&3) and reduce ‘steal’ of portal blood flow.
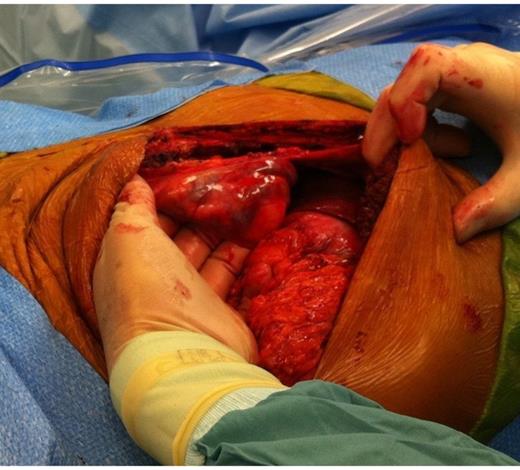
A wedge biopsy of the liver was taken for more thorough histologic evaluation. The lesser sac was entered by dividing the greater omentum, and the omental arcades were interrupted to prevent right-to-left shunting. The right gastroepiploic arcade and the coronary vein were divided to complete the azygoportal disconnection. The pancreas was reflected cephalad and 8cm of splenic vein was skeletonized off the inferior margin of the pancreas by ligature of its perforating branches. The splenic vein was divided flush with the SMV; the latter was repaired in a routine manner. The splenic vein was beveled slightly, turned inferiorly, and then anastamosed to the superior aspect of the left renal vein in an end-to-side fashion with a running posterior suture and interrupted anterior sutures of 6-0 Prolene. Immediate decompression of the portal venous system was evidenced by markedly reduced external abdominal wall varices when closing the abdomen. These continued to diminish in size over the patient’s 5-day postoperative stay, after which he was discharged home and continues to do well at early follow up (Fig 4). Histology of the wedge liver biopsy has since confirmed NRH.

DISCUSSION
This patient presented due to the symptoms of his PH. The 4 mmHg wedge hepatic pressure indicated that his PH was pre-sinusoidal in origin. The aetiology of this presentation was confirmed by wedge biopsy as being NRH. It is interesting that these nodules can be missed on percutaneous liver biopsy and only found from a wedge of tissue taken at surgery (4). Additionally, because the nodules cannot be visualized on routine H&E or trichrome staining, a special reticulin stain must be performed to show the nodules clustered around the portal triads without fibrosis or collagen deposition, in contrast to alcoholic cirrhosis. The pathogenesis of NRH is thought to be a diminution of normal portal blood flow (5). Systemic and portal diseases proposed but not proven to be involved include collagen vascular diseases, myeloproliferative and lymphoproliferative disorders, and autoimmune T-cell response (6,7).
NRH diagnosis consists of ruling out other conditions generating this clinical picture, and management consists of treating sequelae of the resultant PH. Initial medical therapy involves beta-blockade and somatostatin analogues. Esophageal banding and sclerotherapy should be offered to patients with acute hemorrhage from esophageal varices. Long term management requires decompression of the portal venous system. TIPS, commonly employed to emergently decompress PH, is fraught with post-procedural hepatic insufficiency as well as significant rates of stent stenosis (>50%) and thrombosis requiring reintervention (>80%)(8,9). In contrast, the Warren-Zeppa DSRS offers a method for maintaining hepatopetal perfusion while simultaneously decompressing left-sided variceal communications, thereby reducing the risks of both hepatic insufficiency and gastrointestinal bleeding. It is this selective property of the DSRS that sets it apart from other surgical portacaval (central) shunting operations, as well as the more modern angiographically-placed intrahepatic shunts. These procedures rapidly and efficaciously decrease the portal venous pressure, but also reduce hepatic parenchymal flow.
It was noted early in the implementation of the DSRS that patients with this procedure retained a superior ability to handle gastrointestinal protein and ammonia loads, and it is still believed that the relatively high hepatic portal perfusion following DSRS contributes to the lower rates of hepatic insufficiency and encephalopathy(9). Furthermore, DSRS offers remarkably low mortality and reoperative rates, making this operation additionally suitable to patients requiring treatment of PH who have limited follow-up or live in remote areas(10). It is the hope of the authors that familiarity with the DSRS and the indications for its use based upon an understanding of the pathophysiology of PH remain within the lexicon of surgical education. It provides a valuable forum for teaching intricate operative technique, collateralized vascular anatomy, and the pathophysiology of PH-plus it is highly efficacious in treating appropriate patients with portal hypertension.



