-
PDF
- Split View
-
Views
-
Cite
Cite
G Tuyeras, E Pappalardo, S Msika, Acute small bowel obstruction following laparoscopic Roux-en-Y gastric bypass during pregnancy: two different presentations, Journal of Surgical Case Reports, Volume 2012, Issue 7, July 2012, Page 1, https://doi.org/10.1093/jscr/2012.7.1
Close - Share Icon Share
Abstract
Bariatric surgery as laparoscopic Roux-en-Y gastric bypass (LRYGB) is increasing throughout the world and women represent the majority (70%) of patients. Most of them are of reproductive age. As a consequence, surgeons will have to treat more and more pregnant patients with a history of LRYGB for surgical abdominal pain. Reported incidence of small bowel obstruction (SBO) varies from 1.5% to 3.5% after LRYGB including internal hernias, intussusception and volvulus. As two cases of maternal postoperative death have been reported in the literature, diagnosis and surgical treatment shouldn’t be delayed especially during pregnancy. To underline the necessity of a rapid diagnosis and surgical treatment, we reported two cases of severe SBO during pregnancy.
INTRODUCTION
LRYGB is the most common procedure in the surgical treatment of morbid obesity. Women represent the majority (70%) of patients. Small bowel obstruction is a well-known problem after LRYGB caused by internal hernias, intussusceptions or volvulus. Diagnosis is difficult despite aggressive policy. Two cases of maternal postoperative death reported in the literature (1,2) underline the necessity of a prompt surgery.
CASE 1
A 33-year-old woman (gravida 1, para 0) presented to the emergency department (ED) with acute epigastric abdominal pain at 17 weeks gestational age. The pain was associated with nausea and vomiting.
Four year before, she had undergone an antecolic, antegastric LRYGB. For a body mass index (BMI) of 52 kg/m² (126 kg, 1.55 m). When she presented to the ED, her BMI was 34 kg/m² (79 kg). Her early antenatal course had been uneventful. Physical examination revealed normal vital signs, left upper quadrant tenderness without guarding or rebound. A naso-gastric tube was inserted and removed 500cc of biliary liquid. Fetal heart tones and movements were normal.
Intravenous hydration was immediately initiated. No improvement of the pain occurred one hour after non-opioid intravenous sedation; so a laparoscopic diagnosis was decided to evaluate a suspected internal hernia twelve hours after the first symptoms.
At laparoscopy, there was a retrograde intussusception of the proximal common limb into the jejuno-jejunostomy. Dilatation of the biliopancreatic limb was also noticed. The intussuscipien bowel was successfully reduced but had signs of ischemia and a perforation. Through a short laparotomy, a short small bowel resection with a new jejuno-jejunal anastomosis was performed.
At day 2, bowel function started. Her postoperative period was uneventful and she was discharged one week after her surgery without any obstetrical complications.
CASE 2
A 34-year-old woman (gravida 2, para 1) with a 31-week pregnancy presented with abdominal pain. Seven years before, she had undergone a laparoscopic adjustable gastric banding and had lost 56 kg (initial BMI 54 kg/m², weight 139 kg). Unfortunately pouch dilatation occurred 5 years later and the gastric band was removed. After she had a 40 kg weight gain over one year, an antecolic, antegastric LRYGB was performed (BMI at this surgery was 48kg/m², weight 123 kg). Twelve months later, she had lost 43 kg. Her early antenatal course was uneventful. She had a history of midabdominal pain one week before admission; an abdominal computed tomography (CT scan) with oral contrast was performed; a distended proximal small bowel with no specific mention of internal hernia (IH) was noticed and opacification of the colon was obvious.
After 3 days of post-prandial epigastric abdominal pain, nausea, and vomiting, the patient presented once again to the ED. Her vital signs were normal; abdominal examination was consistent with a 31-week gravid uterus but revealed tenderness at the epigastrium without guarding or rebound. The pain was exacerbated by eating and associated with nausea and vomiting. Fetal heart tones and movements were normal. A gastroscopy did not show any ulcer or stenosis at the gastrojejunal anastomosis. The intensity of the pain and the long delay led us to recommend surgery.
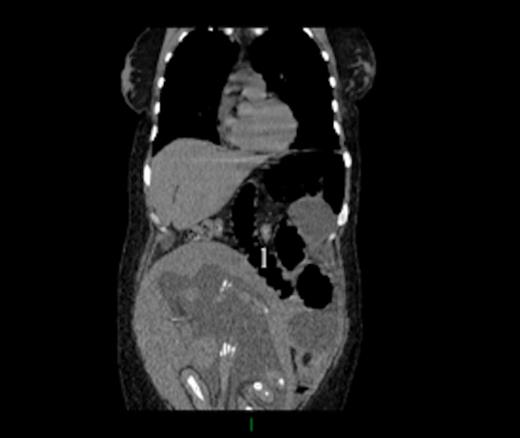
Six days after admission, a laparoscopic evaluation was performed but quickly converted into a laparotomy through a midline incision. An IH of the alimentary limb through the jejunojejunostomy mesenteric defect was found. The herniation was reduced and the strangulated part of alimentary limb was dusky but without frank ischemia. Petersen’s space and the jejuno-jejunostomy mesenteric defects were closed. Four days after surgery, the patient displayed with the same symptoms; a new CT scan (Fig 1) showed a volvulus of the jejunojejunal anastomosis. Re-laparotomy confirmed the CT scan diagnosis. The alimentary limb herniation was reduced and fixed; small bowel resection was not required. Fetal heart monitoring remained normal. Bowel function returned on the second postoperative day, and the remainder of the postoperative period was uneventful. She was discharged one week after second surgery.
DISCUSSION
Acute SBO including IH, volvulus or intussuception is a rare and severe complication after LRYGB during pregnancy. Symptoms are not specific and surgery needs to be performed emergently.
LRYGB is associated with a 5% rate of SBO in some studies (1-9). Incidence of IH can increase in case of rapid excess weight loss, with an incidence nearly twice of obstructive complications. In our two cases, the severity of the SBO could be associated with the pregnancy and the importance of the weight loss.
SBO often occurs during the first pregnancy after surgery (case 1, 2), as in 76% of the reported cases (1-9). Most of the cases occurred during the initial 2 years after surgery when weight loss is mostly achieved. A majority of IH occurs during the third trimester of pregnancy (8). Modification of anatomy due to the growing uterus and the cephalad displacement of the bowel may predispose to IH and volvulus (1). Intussuception is less common. The presence of a jejuno-jejunostomy and a large and rapid weight loss could be linked to the occurrence of intussusception (Case 1).
Radiologic examination represents a challenge: avoiding radiation to the fetus and using this for diagnosis. In these conditions, low-dose CT scan is the examination of choice for this population (10). SBO diagnosis even by CT scan may be misleading. It should be done and analyzed by an experienced radiologist to increase the accuracy of internal hernia diagnosis.
Postoperative mortality is high, around 18% of the reported cases. Most of the reported morbidity and mortality occurred in cases of delay for surgery (over 24 hours). So, even if radiologic diagnosis is not made, surgical exploration is mandatory because of potential life-threatening complications (1).
Clinical signs are not specific but acute abdominal pain after bariatric surgery should not be underestimated. Because of pregnancy, the anatomy and the elasticity of intra-abdominal organs are changed and seem to increase the risk of SBO. Surgery should not be delayed even if radiologic signs are absent, if there is suspicion of SBO. Delay in diagnosis and surgical treatment can expose mother or fetus to death.



