-
PDF
- Split View
-
Views
-
Cite
Cite
P Narh-Martey, M Szuchmacher, M Cicchillo, I Galdyn, Thoracic endovascular aortic repair for thoracic aortic mobile thrombus, Journal of Surgical Case Reports, Volume 2012, Issue 6, June 2012, Page 17, https://doi.org/10.1093/jscr/2012.6.17
Close - Share Icon Share
Abstract
Thoracic aortic mobile thrombus is a rare and significant source of peripheral, visceral, as well as cerebral emboli. A 51-year-old female with a history of emergency left brachial artery embolectomy 5 months previously was referred to our unit for evaluation of a mobile thrombus in the descending thoracic aorta. We describe the successful primary treatment of a symptomatic mobile thrombus in the thoracic aorta by using a stent graft.
INTRODUCTION
The thoracic aortic mobile thrombus is a rare and significant source of peripheral, visceral, as well as cerebral emboli. The diagnosis and management of thoracic aortic mobile thrombus has been variable. We present a case of symptomatic thoracic aortic mobile thrombus, which was successfully managed with a thoracic aortic endovascular stent graft.
CASE REPORT
A 51-year-old caucasian female with a history of emergency left brachial embolectomy 5 months previously was referred to our unit for evaluation of a thoracic aortic mobile thrombus. She has a past medical history of COPD, diabetes mellitus, hypertension, discoid lupus, and schizoaffective disorder and had been on anti-coagulation since her embolectomy. On this presentation she complained of substernal chest pain radiating to the back, which had begun suddenly after one instance of nausea and emesis. Her cardiac enzymes were not elevated and her ECG showed normal sinus rhythm. A cause for her chest pain could not be definitively ascertained and the pain resolved spontaneously.
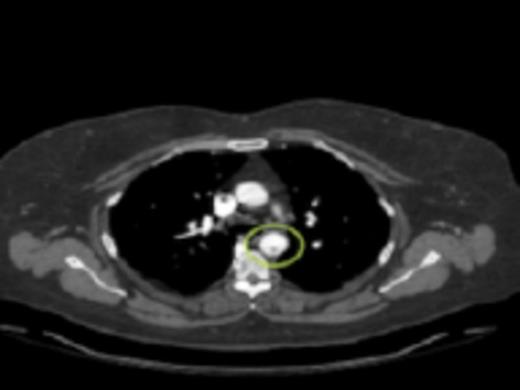
A cross sectional CT-angiogram showing the mobile aortic plaque in the descending thoracic aorta. This image is taken prior to intervention

CTA reconstruction highlighting the floating plaques distal to the Left Subclavian artery takeoff
Initial workup included a transesophageal echocardiogram (TEE) which showed a 0.8cm × 0.9cm highly mobile plaque just distal to the take-off of the left subclavian artery. CT angiography (CTA) was then performed to further delineate the anatomy and to evaluate for the possibility of endovascular stent graft placement. CTA showed a thoracic aortic intraluminal filling defect which represented a small area of clot within an atherosclerotic plaque. The CTA also demonstrated an area of decreased attenuation on the upper anterior portion of the spleen consistent with an older splenic infarct.

Diagnostic aortic angiography demonstrating darkening distal to the left subclavian possibly representing plaque. Image prior to stent deployment
Her past medical history of considerable GI bleeds and her significant fall risk made her a poor candidate for continued anti-coagulation therapy. The appropriateness of the lesion involved and her risk for further embolic events guided selection of endovascular technique for treatment. Exclusion was performed by a 26mm × 10cm thoracic aortic stent graft with balloon angioplasty. Post-procedure angiography confirmed position of the graft distal to the origins of the great vessels and did not demonstrate any leaks. Subsequently, she progressed well and was discharged in stable condition on warfarin and clopidogrel.
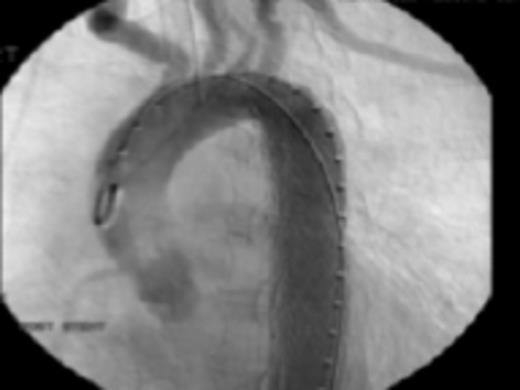
Fig 4: Post endovascular stenting angiography showing appropriate seal without leaks or extravasation of contrast
DISCUSSION
Thoracic aortic mobile thrombus is a rare condition with only approximately 100 cases reported (1). Factors causing aortic thrombi include atherosclerotic lesions, aneurysms, endothelial disorders, and hypercoagulability (2,3,4). Typically, this phenomenon is only diagnosed after symptomatic embolization which prompts a complete workup. In our patient, diagnosis of mobile thoracic aorta thrombus was made following her presentation with a brachial artery thromboembolus. Incidence of thoracic aortic thrombi in cases of peripheral embolism is reported to be as high as 9% (5).
In the case of embolization from an aortic source, recurrent embolization can have dire consequences including loss of limb, splenic infarcts, and cerebrovascular insufficiency. Therefore, therapy should be instituted immediately and directed at prevention of the evolution of atherosclerosis. Multiple strategies have been proposed including initial anticoagulation followed by surgical thrombectomy. Complete disappearance or reduction of thrombus size has also been reported with the use of anti-coagulation alone (1,6). Our patient was given nearly a 5 month-long trial of anticoagulation, which failed to show any improvement in the size of the mobile thrombus as confirmed by serial CTAs. However, the patient's second presentation involving self-resolving atypical chest pain was concerning for further possibilities of embolization. Given the patient's other risk factors, it was important to surgically intervene and prevent a catastrophic embolic event. Surgical intervention allowed us to be sure that entire thrombus was removed and permitted us to be almost certain that no further embolic events would arise from that source. Bowdish et al. came to the conclusion that surgical intervention should be reserved for initial embolic complications and subset of patients who do not respond to anticoagulation therapy. Though our patient received surgical therapy on her second and inconclusive presentation, we believe she adequately fit the second criteria and failed to resolve and even to improve her aortic thrombus on anticoagulation alone.
Thoracic endovascular aortic repair was approved by the FDA in 2005 following a multicenter GORE TAG study (7). One of the most important complications reported by the study was the risk of ischemic stroke. Many further studies have also confirmed the high incidence of ischemic stroke in patients undergoing TEVAR. Care was taken during our procedure to prevent embolization of any atheromatous plaques in the patient's aorta in order to reduce this risk of stroke. Bavaria et al. conducted a prospective study over the course of 8 years looking at the rate of ischemic stroke in patients undergoing TEVAR, which concluded that though refinement of surgical technique was desirable to decrease the risk, it was still preferable to the risk of thromboembolic events associated with mobile thrombi. (8) In our patient, the risk of ischemic stroke had to be weighed against the risk of hemorrhage stroke should the patient be left on anticoagulation and subsequently suffer a fall or a recurrence of her GI bleed. Additionally, endovascular stent graft is also advantageous during simultaneous thrombectomy of lower extremities due to the ability to use a single incision for both procedures. Also, as stated by Fueglistale, et al. the use of ESG treats both the thrombus and the presumed underlying cause of atherosclerotic aortic wall.
Mobile atheromatous plaque of the aorta is a rare medical condition, which lacks a standardized and systemic approach to treatment. Endovascular stent grafting is a suitable method of management with minimal side effects. We describe the successful primary treatment of a symptomatic mobile thrombus in the thoracic aorta by stent graft.



