-
PDF
- Split View
-
Views
-
Cite
Cite
M Garg, S Kumar, S Neogi, Eosinophilic mastitis masquerading as breast carcinoma, Journal of Surgical Case Reports, Volume 2012, Issue 6, June 2012, Page 1, https://doi.org/10.1093/jscr/2012.6.1
Close - Share Icon Share
Abstract
We report the sixth case of Eosinophilic Mastitis, presenting similarly enough to be confused with breast carcinoma. A 50 year old lady presented with a six month history of progressively enlarging asymptomatic breast lump, cough and breathlessness. Clinical examination, mammography and axillary lymphadenopathy suggested malignant disease. Ronchi were heard on chest auscultation. Needle cytology was twice inconclusive and Tru-cut biopsy showed acute on chronic inflammation. Blood investigations revealed significant peripheral eosinophilia. Open biopsy reported eosinophilic mastits, correlating with peripheral eosinophilia and pulmonary symptoms. The patient responded to conservative management. Eosinophilic infiltration of the breast is a rare manifestation of tissue involvement in peripheral eosinophilia. Asthma, Churgh-Strauss Syndrome and hyper-eosinophilic syndromes are associated. Importantly, if a clinically and radiologically malignant breast lump in asthmatic ladies with peripheral eosinophilia is not confirmed on cytology, this entity could be a diagnosis, potentially saving the patient from surgery.
INTRODUCTION
Eosinophilic Mastitis is a very rare entity, confirmed by the fact that, to date only five other cases have been reported in the literature. Expectedly there is scarcity of evidence regarding diagnosis and management strategies but it appears that it is a benign condition, which can be successfully managed non-operatively. This is all the more significant if we realise that most cases have a presentation similar to that of breast carcinoma.
CASE REPORT
A fifty-year-old lady presented to our outpatient department with a painless, progressively enlarging left breast lump of six months duration. There was associated cough and breathlessness for the same duration. There was no history of swelling in the legs, bowel complaints or dermatologic manifestations. No history of urinary symptoms was present. There was no history of loss of weight or loss of appetite. No past history of intake of oral contraceptive pills. The patient was a smoker.
On examination, a swelling of 3 x 6cm was noted in lower outer quadrant of left breast, which was non-tender, hard, mobile and not fixed to overlying skin or chest wall. The nipple-areolar complex was normal and there was no discharge. A 2 x 2cm lymph node of the anterior axillary group was noted. It was firm, non-tender and mobile. No supraclavicular lymph node was present. Bilateral rhonchi were present on chest auscultation. The rest of the examination was unremarkable. Laboratory investigations were unremarkable except for a total leucocyte count of 18000/mm3 (with differential count as P-30, L-20, E-40, M-01) and absolute eosinophilic count-5800 cells/mm3. A p-ANCA screen was negative and bone marrow biopsy was within normal limits. Urine examination was normal and had no evidence of microalbuminuria. Chest X-ray showed nodular opacity in left upper zone likely to be an old solidified granuloma and the rest of lung fields were clear but blunting of left cardiophrenic angle was noted which later showed on ultrasonography to be pleural thickening.
Mammography was done with the provisional diagnosis of malignancy and it showed large ill defined heterodense opacity in retro areolar region of left breast with no evidence of microcalcification hence suggestive of likely malignant etiology. Mammography of right breast was normal.

Fine needle aspiration cytology was done, which twice came back as inconclusive. Then we proceeded for a Tru-cut biopsy, which was reported as predominantly fibroadipose tissue showing moderate mixed acute on chronic inflammation. Only a few benign breast ducts were found that showed periductal fibrosis. No granuloma or atypical cells were identified. Fine needle aspiration cytology of left axillary lymph node showed only reactive lymphadenopathy.
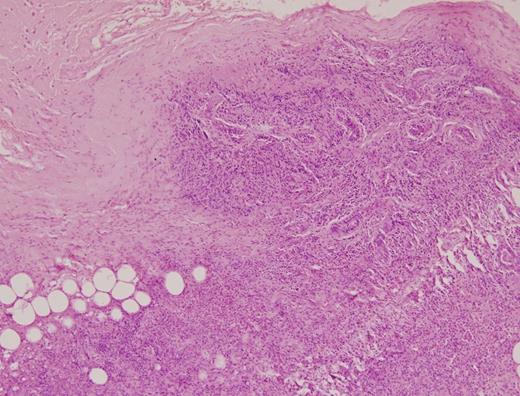
In view of the fact that Triple assessment of the breast lump was not conclusive either for carcinoma or ruling it out all together, open biopsy was undertaken. Biopsy revealed diffuse and dense periductal and stromal inflammatory infiltrate comprising sheets of plasma cells, large number of eosinophils, scattered foamy histiocytes and some lymphocytes. There was diffuse stromal fibrosis and no cells suggestive of malignancy were seen. The diagnosis of eosinophilic mastitis was suggested.
A correlation was established between patient’s pulmonary symptoms and breast lesion. She was started on oral and inhalational steroids in consultation with our internal medicine colleagues. The patient showed an excellent response to this treatment within fifteen days. Complete clinical and radiological resolution of her breast lesion was documented on follow up two months later.
DISCUSSION
Eosinophilic Mastitis describes a condition of tissue eosinophilia confined to the breast. Tissue eosinophilia is usually accompanied by peripheral eosinophilia reflected by a high eosinophil count both absolute and in the differential leucocyte count. There are many known causes for peripheral eosinophilia such as inflammatory allergic diseases, parasitic infestations, collagen diseases and haematological malignancies. Breast tissue, however remains a rare location for tissue eosinophilia to manifest and to date, of the five cases reported so far, the distribution of associated diseases is as follows (1-5). Two were asthmatic, two were diagnosed to have Churg-Strauss syndrome and one had hyper-eosinophilic syndrome.
Our patient started having symptoms of breathlessness coinciding with the onset of her breast lump. On further evaluation by our internal medicine colleagues with the histopathological report in hand, a collaborative diagnosis of Asthma was made, further substantiated by the excellent response shown to inhalation steroids. This lady also had a significant peripheral eosinophilia unresponsive to anti parasitic chemotherapy, a normal bone marrow biopsy aspirate and p-ANCA, which was non reactive thus ruling out parasitic infestations, collagen diseases such as Churgh-Strauss Syndrome and haematological malignancies.
The important aspect of this case was the fact that clinically and radiologically malignant appearing breast lumps in asthmatic ladies having peripheral eosinophilia but not proved on FNAC or Tru cut biopsy should trigger a high index of suspicion in the minds of both the surgeon and pathologist regarding this rare condition as a positive diagnosis could potentially save the patient from mutilating radical surgery.



