-
PDF
- Split View
-
Views
-
Cite
Cite
R Subash, ML Arunkumar, VA Iyoob, N Bonny, Inflammatory myofibroblastic tumour of liver masquerading as hilar cholangiocarcinoma, Journal of Surgical Case Reports, Volume 2011, Issue 8, August 2011, Page 7, https://doi.org/10.1093/jscr/2011.8.7
Close - Share Icon Share
Abstract
There is a wide variety of inflammatory and benign neoplastic disorders of the biliary system that mimic cholangiocarcinoma in terms of clinical manifestations and imaging findings. Inflammatory myofibroblastic tumour of the bilary tract is one such condition, which is extremely rare but benign. Like cholangiocarcinoma this condition presents as painless progressive obstructive jaundice and it is often difficult to differentiate between the two prior to laparotomy, with the usual investigative modalities. Diagnosis is usually established by the characteristic histopathology findings in biopsy specimen. Newer diagnostic modalities directed at obtaining preoperative biopsy of the lesion appear promising in differentiating benign from malignant biliary lesions, but their routine use is yet to become standardised. Until then, awareness of doctors about the existence of such benign entities might prompt a less aggressive treatment approach while dealing with atypical hilar lesions of liver.
INTRODUCTION
Inflammatory myofibroblastic tumour (IMFT) or inflammatory pseudotumor of the biliary tract is an extremely rare benign disease(1). The clinical manifestations and imaging features of this lesion are similar to the malignant neoplasms of the biliary tree. Hence the diagnosis is most often a postoperative histological surprise (2). We present a case of inflammatory pseudotumour of the hilar region which mimicked Klatskin tumour or hilar cholangiocarcinoma (CCA).
CASE REPORT
21 year old female patient presented with painless progressive jaundice of one month duration. She had generalized pruritus, severe loss of weight and loss of appetite. She had no other co-morbidity. On examination she had icterus and hepatomegaly. Laboratory investigations revealed evidence of obstructive jaundice with serum total bilirubin of 16 mg/dL and conjugated bilirubin 8.2 mg/dL. Other abnormal findings included elevations in serum alkaline phosphatase (789 IU/L), ALT (61 IU/L) and AST (40 IU/L). Tumour markers in the serum showed a mild rise in CA 19-9 (45 U/ml) whilst both AFP (4 ng/ml) and CEA (1.4 ng/ml) were within normal limits. Hepatitis serology (HBSAg and anti HCV) and HIV status were negative. Ultrasound revealed a collapsed gallbladder with bilateral intra hepatic biliary radical dilatation and a suspicious lesion at the hilum of liver. Subsequent MRI with MRCP (Figure 1) showed a definite lesion in the confluence of right and left major bile ducts with extension in to the left duct to involve secondary biliary radicles on that side, consistent with Type-3b Klatskin tumour according to Bismuth classification. The lesion was hypo-intense in T2, FIESTA and LAVA sequences of MRI and it showed moderate enhancement in venous phase. With the diagnosis of hilar CCA, patient was taken up for surgery after preoperative optimisation.
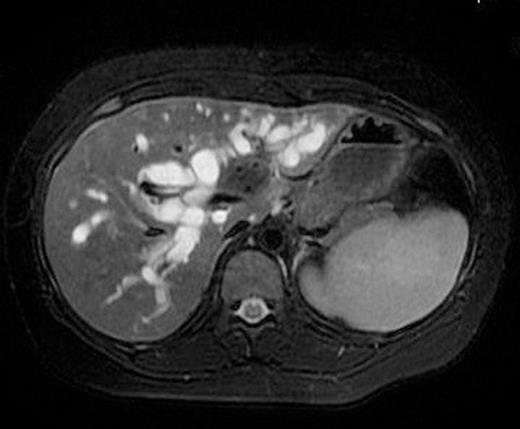
MRI of the liver showing lesion at the confluence of right and left hepatic ducts with extension in to the left duct.
Intra-operatively a lesion was seen at the hilum of liver with extension into left lobe. The tumour was found to be infiltrating a small portion of common hepatic artery and main portal vein. So patient underwent left hepatectomy, caudate lobe excision and radical bile duct excision along with excision and reconstruction (with interposition autologous vein graft) of the involved portion of portal vein and hepatic artery.
On cutting through the hilum, an ill circumscribed grey white firm to hard area was identified macroscopically involving the confluence of right and left bile ducts with extension of the lesion into left liver. Microscopically the lesion was composed of fascicles of spindle cells including fibroblasts and myofibroblasts and collections of plasma cells and lymphocytes. On immunohistochemistry, myofibroblasts showed positivity with Smooth Muscle Actin, and were negative for Cytokeratin and S100. Thus a histopathology diagnosis of inflammatory myofibroblastic tumour of hilar region of liver was given.
DISCUSSION
Klatskin tumor, or hilar CCA involving the bifurcation of the hepatic duct, accounts for approximately 60 % of all bile duct cancers and is the second most common primary malignant hepatobiliary neoplasm. Diagnosis and treatment of Cholangiocarcinoma is challenging and the prognosis is uniformly poor, with only 20 to 25% of patients surviving 5 years after surgical resection. A wide spectrum of neoplastic and nonneoplastic conditions of the biliary tract, mimicking cholangiocarcinoma, adds to the complexity of management (3). In most cases, a definitive diagnosis can be established only with histopathology examination of the biopsy specimen. Indeed, in a large surgical series (4), 24% of resected specimens showed benign disease in patients undergoing surgery for presumed hilar cholangiocarcinoma.
Inflammatory myofibroblastic tumour is an idiopathic benign mass lesion composed of fibrous tissues, myofibroblasts and marked inflammatory infiltration, predominantly plasma cells. The most common sites of involvement are the lungs, mesentery and omentum. Other sites include soft tissue, mediastinum, GIT, pancreas, genitourinary system, oral cavity, skin, breast, nerve, bone, CNS, salivary glands, etc. Inflammatory myofibroblastic tumour involving biliary tract is rare. It usually occurs in children and young adults. The clinical and imaging features of this lesion are similar to those of a neoplasm, and the biological behavior and the property of spontaneous regression suggest a benign nature (5). But there are several reports of its association with antecedent infections and so some consider IMFT as a non-specific chronic inflammatory lesion. Epstein-Barr virus has been found within the lesion in some IMFTs, particularly in the liver (6). Microscopically, IMFT is characterized by plenty of inflammatory infiltrates consisting of predominantly lymphocytes, plasma cells and histiocytes, admixed with a variable proportion of fibroblasts and myofibroblasts (7). On immunohistochemistry tumour cells exhibit strong diffuse positivity with smooth muscle actin, and are negative for cytokeratin and S100 (7).
Clinically IMFT presents with progressive obstructive jaundice, abdominal pain, fever, anaemia and features which are indistinguishable from biliary tract malignancy (8,9). Tumour markers like CA 19-9 may be elevated in both CCA and IMFT. Imaging appearance also may be deceiving as IMFT presents with mass lesions, biliary radical dilatations, infiltrations and even delayed and persistent enhancement with contrast (due to its fibrous content) which are strikingly similar to CCA (2). Several authors have tried to differentiate this lesion using different modalities like CECT, MRI and PET-CT; but without much help (2). Brush cytology of the biliary lesion using ERCP or PTC is often undertaken, but the diagnostic yield is poor. Newer techniques such as intraductal ultrasound and cholangioscopy have been used to obtain direct biopsy specimens, but their clinical benefits are yet to be proven (10). Use of intraoperative frozen section biopsy, meticulously evaluated by an expert pathologist may be of some help in planning the extent of resection.
We reported this case to emphasise that, though most tumours arising at the hepatic duct convergence are malignant, benign lesions are also encountered. Hepatobiliary surgeons and radiologists should keep this in mind, so that the possibility of a benign lesion is considered pre-operatively in atypical cases and every effort is made to rule out this lesion before embarking on aggressive surgical procedures.



