-
PDF
- Split View
-
Views
-
Cite
Cite
Jonathan Yin, Anthony Marino, Peter Cooke, Khaldoun Bitar, Post-radiotherapy vesicocutaneous fistula presenting as gas/fluid-filled groin swelling, Journal of Surgical Case Reports, Volume 2011, Issue 6, June 2011, Page 4, https://doi.org/10.1093/jscr/2011.6.4
Close - Share Icon Share
Abstract
We report an interesting and rare case of a vesicocutaneous fistula, which was diagnosed only one year following radiotherapy. A 71 year old gentleman presented with a gangrenous swelling of his left thigh. A copius amount of urine was seen to be draining from the site after initial incision and drainage. Computed tomography with contrast confirmed the diagnosis of a vesicocutaneous fistula. Bilateral nephrostomies were inserted to aid spontaneous closure of the fistula. Previous case reports of vesicocutaneous fistulae involving radiotherapy have described the complication of a fistula occurring many years after the intervention.
INTRODUCTION
A vesicocutaneous fistula is a tract that forms a connection between the bladder and the skin, and is most commonly associated with a suprapubic cystostomy tract that fails to close. (1) Other reported causes of this type of fistula include pelvic trauma and following pelvic surgery. (2,3,4) Vesicocutaneous fistulae have also been reported following unrecognized bladder rupture, after bladder repair, and secondary to bladder calculi. (2,5,6) To the best of our knowledge, there have only been two previous reported cases of vesicocutaneous fistulae occurring post-radiotherapy. (7,8) We report the unusual and rare case of a patient diagnosed with a vesicocutaneous fistula one year post-radiotherapy; discussing the presentation and management options.
CASE REPORT
A 71 year old gentleman was referred urgently by his GP with a lump in his left upper thigh.
It had been noted several months earlier; an ultrasound scan suggesting a haematoma. It had slowly enlarged but had now become increasingly painful in the preceding 24 hours.
Background history revealed that he had undergone an uncomplicated laparoscopic radical prostatectomy for prostate cancer in 2008 and radiotherapy in 2009. He had subsequently developed a bladder neck stenosis, which was treated with bladder neck incision/dilatation but he still required daily self-catheterisation.
On examination, the patient was found to be drowsy and lethargic but remained co-operative, and his observations showed him to be afebrile and haemodynamically stable. A tender, tense 5 x 10cm swelling was noted in the anterior femoral triangle of his left thigh. The overlying skin appeared necrotic with surrounding erythema, palpation revealing surgical emphysema.
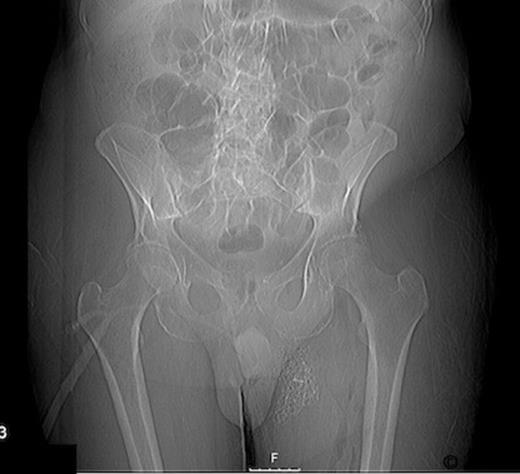
Radiographs confirmed subcutaneous gas associated with the swelling (figure 1). The patient was consented for incision and drainage of the collection, where it was noted that gas bubbles were released on initial stab incision. Copious grey watery fluid was drained from the cavity which appeared to track under the inguinal ligament. Cavity fluid and biopsy specimens were sent for microscopy, culture and sensitivity. The cavity was packed and broad spectrum antibiotics were started following consultation with a microbiologist. A pelvic CT scan with contrast was arranged (figure 2–4), which confirmed a vesicocutaneous fistula.
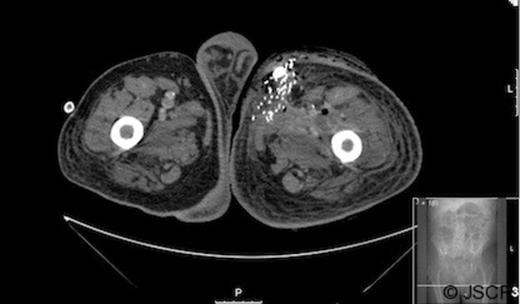
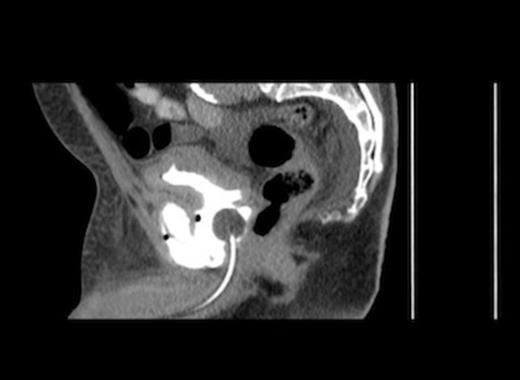
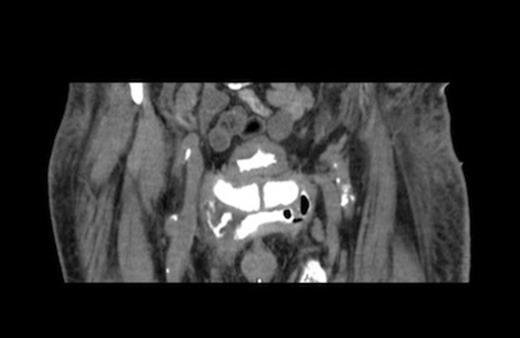
Figures 2, 3, and 4 are axial, sagittal, and coronal views, respectively, of computed tomography with contrast introduced by urinary catheter. This CT cystogram shows a leak/fistula at the low anterior bladder wall. The fistula has a communication with the pubic symphysis and a collection lies anterior to this. The tract extends distally, communicating with the cavity in the left anteromedial aspect of the thigh.
Frequent change of wound packing/dressings were required suggesting a high (volume) output urinary fistula. Bilateral nephrostomies were required for temporary urinary diversion to allow spontaneous closure of the fistula. The closure of the thigh wound by secondary intention was aided by the use of a negative pressure (sponge) dressing system.
DISCUSSION
To the best of our knowledge, the only previous reports of a vesicocutaneous fistula post-radiotherapy include a case report by Lau et al, describing the sequelae of the fistula in a patient who had suffered vulval cancer. (7) The tumour was deemed unresectable and radiotherapy was administered. Two years later, she was found to have a vesicocutaneous fistula presenting as right groin pain. The only other case prior to this involves a case with the diagnosis of the fistula being ten years post-radiotherapy. (8)
The patient in our case report was diagnosed with a vesicocutaneous fistula following the presentation, operative findings, and imaging provided. Gas gangrene and necrotising fasciitis were also initially considered, and so a broad spectrum antibiotic (meropenem) was given following consultation with a microbiologist. Staphylococcus aureus (9), a well recognised gas forming organism, was subsequently isolated from the operative specimens.
The patient was initially diagnosed with prostate cancer and treated with radical prostatectomy in 2008. The histology confirmed moderately differentiated adenocarcinoma. In 2009, he suffered biochemical failure (rising PSA) and salvage radiotherapy was administered to the prostate bed in a dosage of 66 Gray in 33 fractions. He developed bladder neck stenosis which was treated with endoscopic incision/dilatation and the patient was taught self-catheterization techniques.
Only one year after receiving radiotherapy, as described in the case report, the patient presented to our hospital, where the complication of a vesicocutaneous fistula was diagnosed. The case is also unusual because classically, a fistula occurs where there is distal obstruction but in our patient, the bladder neck stenosis had resolved. The fistula was not obviously related to intermittent self- catheterisation as its site was away from the urethro-vesical anastomosis (bladder neck).
When considering the management of a vesicocutaneous fistula in a patient who is post-radiotherapy, tissue viability is always a concern because post-operative healing may be affected. (10) Fistulectomy/partial cystectomy has been described but was not required in this case. (5) Factors affecting the closure of the external wound must also be taken into account. Closure may be prevented by a high-output fistula and recurrent infections. Therefore, a urinary diversion system and appropriate wound care is essential to allow spontaneous closure of the fistula. Bilateral nephrostomies were required for temporary urinary diversion in our patient to allow for spontaneous closure of the fistula. The closure of the thigh wound by secondary intention was aided by the use of a negative pressure (sponge) dressing system.



