-
PDF
- Split View
-
Views
-
Cite
Cite
S Sadhu, S Sarkar, R Verma, SK Dubey, MK Roy, Haemosuccus pancreaticus due to true splenic artery aneurysm: a rare cause of massive upper gastrointestinal bleeding, Journal of Surgical Case Reports, Volume 2010, Issue 5, July 2010, Page 4, https://doi.org/10.1093/jscr/2010.5.4
Close - Share Icon Share
Abstract
“Haemosuccus pancreaticus” is an unusual cause of severe upper gastrointestinal bleeding and results from rupture of splenic artery aneurysm into the pancreatic duct. More commonly, it is a pseudoaneurysm of the splenic artery which develops as sequelae of pancreatitis. However, true aneurysm of the splenic artery without pancreatitis has rarely been incriminated as the etiologic factor of this condition. Owing to the paucity of cases and limited knowledge about the disease, diagnosis as well as treatment become challenging. Here we describe a 60-year-old male presenting with severe recurrent upper gastrointestinal bleeding and abdominal pain, which, after considerable delay, was diagnosed to be due to splenic artery aneurysm. Following an unsuccessful endovascular embolisation, the patient was cured by distal pancreatectomy and ligation of aneurysm.
INTRODUCTION
Haemosuccus pancreaticus is a rare and potentially life threatening clinical entity, and is described as bleeding from the ampulla of Vater via the pancreatic duct. The syndrome is classically attributed to erosion of the splenic artery aneurysm in to the pancreatic duct or bleeding in to a pseudopancreatic cyst as a result of acute or chronic pancreatitis causing intermittent severe upper gastrointestinal (GI) bleeding. However, haemosuccus pancreaticus due to true splenic artery aneurysm without pancreatitis is an extremely rare condition. In addition, relative lack of knowledge and rarity of the disease makes the diagnosis even more challenging. Here we present a case of hemosuccus pancreaticus due to true splenic artery aneurysm.
CASE REPORT
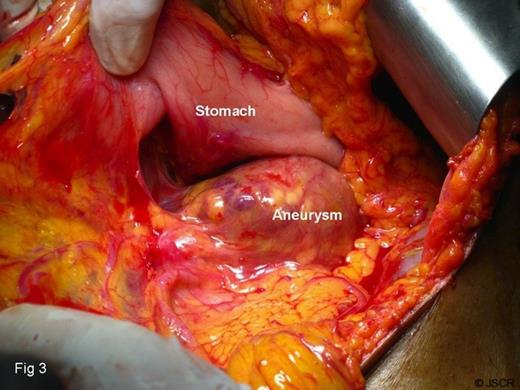
A 60-year-old male was referred with history of repeated epigastric pain and malena. The pain was intense, radiated to the back and, on occasion was associated with profuse sweating and fainting attacks. In the preceding four months, he had 5 such episodes of pain and malena. These attacks were characterized by malena occurring a few hours after the onset of pain and were associated with transient elevation of serum amylase and lipase. He was a known hypertensive on regular medicines and denied any history of alcohol consumption. During the last episode of bleeding, his hemoglobin had dropped to 3.5gms/dl requiring 8 units of blood transfusion. Upper GI endoscopy performed on three occasions showed bleeding from the second part of the duodenum, but the source of bleeding remained obscured. Colonoscopy at the time was unremarkable. In view of suspected pancreatitis, abdominal ultrasonography was performed, which revealed a hypo-echoic lesion near the head-neck junction of pancreas. On contrast CT scan, this lesion turned out to be a partially thrombosed 7cm aneurysm close to an otherwise normal pancreas (Fig.1). The 3D-CT reconstruction clearly demonstrated the origin of the aneurysm to be from the splenic artery (Fig.2). To stem further bleeding, a coeliac axis angiography followed by micro-coil embolisation of splenic artery was performed.

Contrast CT shows partially thrombosed splenic artery aneurysm. ( A =aneurysm, SA =splenic artery, CA =celiac artery, P =pancreas)
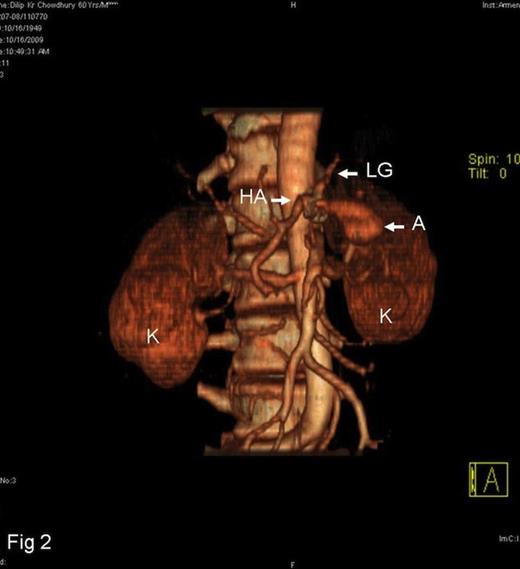
3D-CT reconstruction of the aneurysm ( HA =hepatic artery, LG =left gastric artery, A =aneurysm, K =kidney)
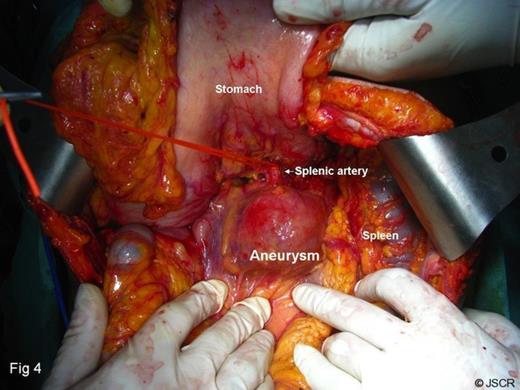
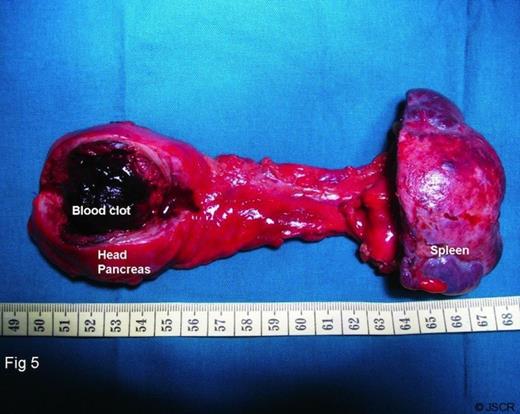
Three weeks after the embolisation, the patient represented with the severe malena and abdominal pain necessitating laparotomy. This revealed a fairly large aneurysm abutting the postero-superior aspect of the head-neck region of the pancreas, while rest of the pancreas appeared and felt normal (Fig. 3). As a result of the embolisation, the spleen was infarcted at places with adhesions between its outer surface and the diaphragm. Dissection revealed the aneurysm to be arising from splenic artery, which was ligated and excised en block with distal pancreas and spleen (Fig.4, Fig.5). Post operative histology demonstrated a normal pancreas and an atherosclerotic aneurysm. The patient had an uneventful recovery and was symptom free at 3-month follow up.
DISCUSSION
The term “haemosuccus pancreaticus” was coined by Sandbloom in 1970 upon discovery of three cases of bleeding pancreatic duct. (1) Until now, approximately 100 cases of haemosuccus pancreaticus have been reported in the literature.(2) Splenic artery aneurysm following pancreatitis (pseudoaneurysm), and bleeding into a pseudopancreatic cyst remain the principal causes of this condition.(3) Rarely, pseudoaneurysm of other peripancreatic vessels like hepatic artery,(4) celiac artery (2) and gastroduodenal artery (5) erodes into the pancreatic duct causing haemosuccus pancreaticus. However, haemosuccus pancreaticus without pancreatitis is extremely rare, and to our knowledge, 23 such cases due to true splenic artery aneurysm have been reported since 1931.(6)
Atherosclerotic splenic artery aneurysm is primarily a disease of elderly age group (mean 60) with a striking male predominance (M:F=8:1). Majority of patients present with classic symptoms of severe recurrent upper GI bleeding and sharp epigastric pain.(1) In addition, there is an unusual correlation between the pain and bleeding, with the former invariably preceding bleeding. Severe anaemia, fainting attack or hypovolaemic shock due to bleeding into the pancreatic duct often leads to repeated emergency admission and resuscitation. Such patients often develop transient jaundice along with hyperamylasaemia and/or hyperlipasaemia due to the blockage of pancreatico-biliary system by the blood clots and such was the situation in this patient (6). The diagnosis is established by demonstration of bleeding from the ampulla of Vater during an endoscopy. However, due to the typical intermittent nature of the bleeding, reported success is only 33% by this method. Nevertheless, presence of blood clots in the 1st or 2nd part of duodenum is an indirect evidence of the disease (7). Contrast CT scan and coeliac axis angiography are important diagnostic tools for the characterisation of the aneurysm as well as demonstrating its communication with the pancreatic duct, but in this patient, no communication between the aneurysm and duct could be established.
At present, there is no standardised treatment protocol for haemosuccus pancreaticus due to true splenic artery aneurysm. The bleeding could be controlled by endovascular embolisation, and a high success rate (79%) has been reported for visceral artery aneurysm.(8) However, such a procedure failed in this patient, presumably due to the large size of aneurysm. Surgery in the form of ligation of splenic artery proximal to the aneurysm along with some form of pancreatectomy is curative, an option which proved life saving in this patient (7).
Haemosuccus pancreaticus should be suspected in patients presenting with upper GI bleeding and severe abdominal pain with apparently normal upper GI endoscopy. While contrast enhanced CT scanning can ultimately be conclusive, abdominal ultrasonography, otherwise not a very useful investigation to evaluate upper GI bleeding, can prove useful in the diagnosis of this rare condition.



