-
PDF
- Split View
-
Views
-
Cite
Cite
Arthur Yushuva, Michael McMahon, Elliot Goodman, Transoral incision free fundoplication (TIF) – A new paradigm in the surgical treatment of GERD, Journal of Surgical Case Reports, Volume 2010, Issue 5, July 2010, Page 1, https://doi.org/10.1093/jscr/2010.5.1
Close - Share Icon Share
Abstract
An estimated 10 billion dollars is spent treating gastro-oesophageal reflux disease (GERD) in the USA every year. The present article reports a case of the safe and successful use of transoral incisionless fundoplication (TIF) using the EsophyX90™ device in the surgical treatment of GERD.
INTRODUCTION
GERD is usually characterized by symptoms caused by esophageal mucosal exposure to acidic gastric contents. The pathophysiology is related to failure of the lower esophageal sphincter (LES) to act as a barrier to gastric reflux. The adequacy of LES function is dependent on its pressure, total length and portion exposed to positive intra-abdominal pressure. Defects in one or a combination of the above factors will lead to reflux. (1) The prevalence of GERD has been increasing for the last 2 decades. (2) It affects 10-20 % of the adult population in the developed world, with its highest prevalence in North America. An estimated 10 billion dollars is spent treating GERD in the USA every year. (2)
Treatment of GERD begins with lifestyle modifications. Proton pump inhibitors (PPIs) have been shown by multiple randomized controlled trials (RCT) to be the most effective medical therapy for GERD. Several large meta-analysis of multiple RCT showed that PPIs are superior to histamine 2 receptor blockers (H2RB) in short term treatment of esophagitis and long term maintenance therapy to prevent symptomatic relapse and endoscopicaly proven esophagitis. (3,4)
Most patients with GERD are well controlled with medical management. However, surgery should be considered in patients with progressive disease, extraesophageal symptoms, and GERD-related complications such as strictures or Barrett's esophagus. It should also be considered in younger patients intolerant of PPIs or post menopausal female patients at risk for fractures due to PPI-induced calcium malabsorption.
Laparoscopic Nissen fundoplication, which involves a 360 degree wrap of the gastric fundus around the esophagus at the gastro-esophageal junction, is the current surgical procedure of choice for severe, refractory GERD. Studies have shown over 90 % success in symptom resolution, improved quality of life and overall improvement of general health in over 70 % of patients. Reoperation for symptoms of heartburn, dysphagia, bloating and inability to belch due to disruption or slippage of a fundoplication has been reported in up to 7% of patients after laparoscopic Nissen fundoplication. (5)
CASE REPORT
The patient was a twenty nine years old male with long standing Gastro-Esophageal Reflux Disease (GERD) who had been treated with high dose proton pump inhibitors (PPIs) for over 3 years with little response. He presented for surgical consultation. The patient complained of symptoms of heartburn gradually progressing to throat pain, ear pain and tinnitus. Symptoms would worsen when laying supine, after a large meal and with specific foods such as chocolate, spicy foods and alcohol. The patient had some relief of his symptoms with PPIs initially but then the symptoms recurred.
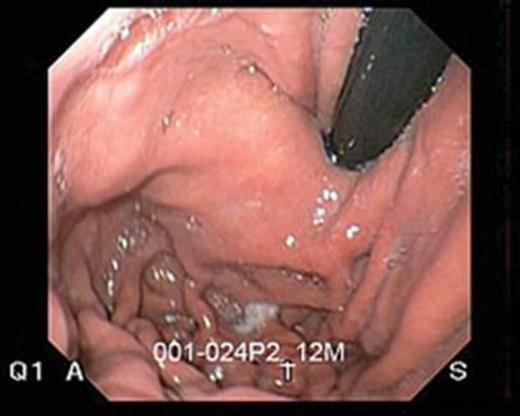
Pre-operative upper endoscopy showed a Hill grade I gastro-esophageal valve, (Fig. 1) grade A esophagitis and normal gastric and duodenal mucosa. Urease test was negative for Helicobacter pylori. Motility study showed only 25% of swallows produced peristaltic wave throughout the esophagus with a mean distal amplitude of 77mmHg. The remaining swallows produced a mixture of low amplitude synchronous waves, partially propagated and non-propagated waves. The lower esophageal sphincter (LES) measured to 3 cm, with 1 cm above the diaphragm. The LES had a mean resting pressure of 9 mmHg, which relaxed with swallowing. A twenty four hour pH study produced a deMeester score of 20.25 (normal range below 14.5).

The patient elected to undergo a transoral incision-less fundaplication, in which a 4 cm gastro-esophageal valve was created after the endoscopic application of 14 polypropylene transmural fasteners through the gastric fundus and the distal esophagus (1-3 cm above the Z-line). The procedure also produced a 270 degree endoluminal wrap of the fundus around the intra-abdominal esophagus. (Fig 2) The total operative time was 75 minutes. There were no major intra-operative complications, minimal intra-operative blood loss and the patient was discharged home the morning after surgery.
Early after surgery, the patient complained of throat pain and abdominal bloating. These complaints, however, soon resolved. Two months after the procedure, the patient's symptoms of reflux had significantly resolved. He was almost completely off his PPIs, he could eat many of the foods which gave him reflux before surgery without any difficulty and he could now sleep lying flat, something which he had been unable to do for three years.
DISCUSSION
A novel approach in the evolution of the surgical treatment of GERD is the transoral incisionless fundoplication (TIF). TIF employs a tissue plication device called EsophyX (EndoGastric Solutions, Redmond, WA, USA) that endoscopically replicates a 270-320 degree gastric fundoplication to create a 3-4cm neo-valve at the GE junction. The procedure is done under general anesthesia, with either oro-tracheal or naso-tracheal intubation, with the patient positioned in either the left lateral decubitus or supine position on the operating table. The operating team consists of an endoscopist who provides continued retroflex visualization of the GE junction and a second operator, usually a surgeon, who performs the actual tissue manipulation and plication.
After a single transoral introduction of the instrument over the endoscope, the gastric fundus is retracted by a helical retractor. This creates a 3-4 cm long sleeve of tissue that is plicated by 6mm H-shaped polypropylene fasteners in a 200 to 300 degree fashion. Full thickness serosa-serosa plication at 1-2 cm above the gastro-esophageal junction begins with deployment of fasteners at the posterior and anterior side as visualized with the endoscope in the retroflexed view. Plication then continues at the greater curvature, 3-4 cm above the gastro-esophageal junction as the tissue is being pulled down. (Fig 3) By the end of the procedure (which typically takes 45-75 minutes), TIF increases the length of intra-abdominal esophagus, reduces small hiatal hernias, creates a 3-4cm GE valve and recreates the angle of His.
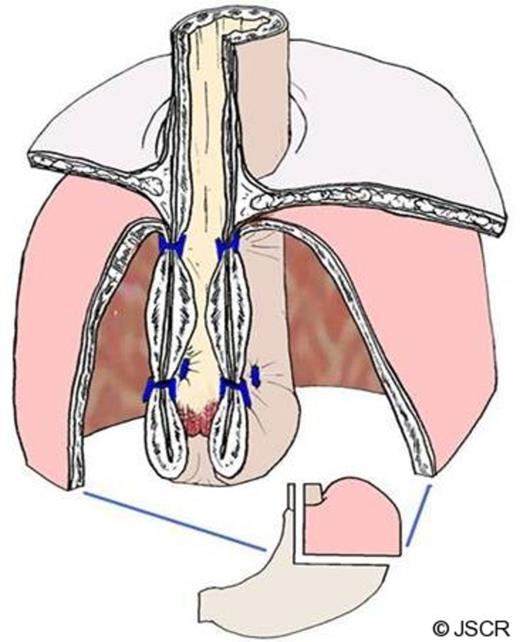
Full thickness serosa-serosa plication at 1-2 cm and 3-4 above the gastro-esophageal junction.
The performance of TIF with EsophyX has been FDA approved in the USA since September 2007. Over the last 2 and half years, 2000 cases have been performed in the USA. A further 1000 cases have been performed in Europe. The efficacy of the procedure has been reported in several studies. Cadiere and his group were able to show no adverse effects, greater then 50% improvement in GERD-HRQL scores, elimination of heartburn in 93% of patients, PPI use in 71% of patients and esophagitis in 55% of patients at 2 year follow up. (6) Newer unpublished data from two case series (n = nearly 70 patients) from two independent investigators in United States demonstrate normalization of esophageal pH in 76 % of patients and complete independence from PPI's in approximately 90% of patients. 87% of subjects were satisfied and 82% were asymptomatic based on HRQL and GSRS scores.
Complication rates are low after TIF. Early on in the European experience, three patients sustained non-lethal esophageal perforations during passage of the EsophyX device. No further cases of perforation have been reported since. Intra-operative bleeding requiring blood transfusion is very uncommon.
TIF with EsophyX is effective in decreasing symptom severity, daily PPI requirements and improving quality of life (in the short term) in patients with moderate to severe GERD. TIF can also reduce small (<2cm) hiatal hernias. TIF with EsophyX successfully increases LES resting pressure, decreases acid reflux and supports esophageal healing in chronic GERD. TIF with EsophyX is less invasive than its laparoscopic counterpart. Long term studies are needed to establish whether it is will be as durable as more traditional forms of anti-reflux surgery.



