-
PDF
- Split View
-
Views
-
Cite
Cite
M West, PSV Prasad, G Ampat, New onset epilepsy following unintentional durotomy in a patient on anti-psychiatric medication, Journal of Surgical Case Reports, Volume 2010, Issue 2, April 2010, Page 3, https://doi.org/10.1093/jscr/2010.2.3
Close - Share Icon Share
Abstract
We would like to present a rare case report describing a case in which new-onset tonic-clonic seizures occurred following an unintentional durotomy during lumbar discectomy and decompression. Unintentional durotomy is a frequent complication of spinal surgical procedures, with a rate as high as 17%. To our knowledge a case of new onset epilepsy has never been reported in the literature. Although dural tears during surgery and CSF hypovolaemia are thought to be the main contributing factors, one postulates on the effects of anti-psychiatric medication with epileptogenic properties. Amisulpride and Olanzapine can lower seizure threshold and should be used with caution in patients previously diagnosed with epilepsy. However manufacturers do not state that in cases where the seizure threshold is already lowered by CSF hypotension, new onset epilepsy might be commoner. Finally, strong caution and aggressive post-operative monitoring is advised for patients with CSF hypotension in combination with possible epileptogenic medication.
INTRODUCTION
Unintentional durotomy is a frequent complication of spinal surgical procedures, with a rate as high as 17% (1). A small percentage of patients with unintentional durotomy sustain intracranial haemorrhage, likely due to an alteration in intradural hydrostatic dynamics caused by cerebrospinal fluid hypovolaemia. Despite the gravity of this complication, to our knowledge, only a few cases have been previously documented. To our knowledge a case of new onset epilepsy has never been reported in the literature.
The purpose of this report is to describe a case in which new-onset tonic-clonic seizures occurred following an unintentional durotomy during lumbar discectomy and to discuss the importance of our findings in relation to the possible pathophysiological mechanisms.
CASE REPORT
A 62 year old female presented to a spinal orthopaedic clinic complaining of pain in the anterior aspect of her right thigh for at least a year. She could only walk for 15 minutes, thus this limited the patient’s activities of daily living. Medical history was unremarkable but for bipolar depression which was treated by electroconvulsive therapy and anti-psychiatric medication. Her drug history includes Amisulpride, Lorazepam, Olanzapine and Paroxetine.
Magnetic Resonance Imaging scan (Fig. 1–4) showed L2/3 disc prolapse impinging on the right exit canal and causing L2 and L3 compression, thus she was listed for L2/3 lumbar discectomy and decompression. Examination of the right L2/L3 dermatomes revealed severe paresthesia and mild grade 4/5 weakness; reflexes were all normal. All other neurological examination was normal.

Preoperative sagittal T1 weighted image showing disc bulge at L2/3
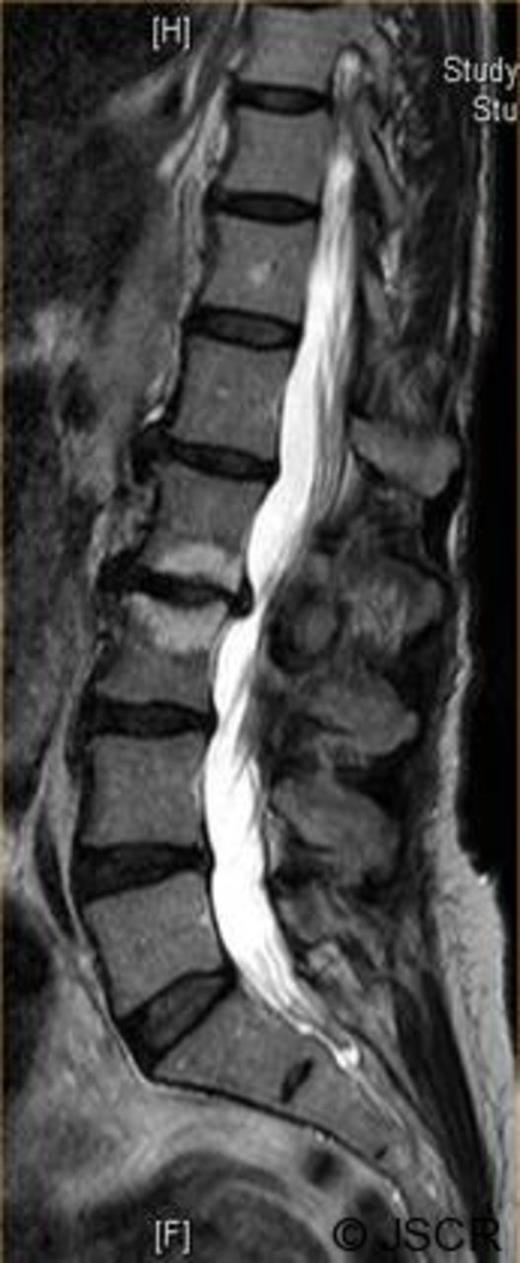
Preoperative sagittal T2 weighted image showing disc bulge at L2/3
Elective bilateral L2/L3 lumbar discectomy and L2/L3 decompression was performed. Access was achieved via a posterior midline incision and tissue dissection was carried out. Decompression was carried out bilaterally with preference to the right. On the right both exiting and traversing nerve root canals were decompressed.

Preoperative axial T1 weighted image showing disc bulge at L2/3 to the right.

Preoperative axial T2 weighted image showing disc bulge at L2/3 to the right.
During dissection, an unintentional dural tear was made, resulting in a loss of cerebrospinal fluid. This was primarily sutured and covered with DuraGen (Integra LifeSciences, Plainsboro, New Jersey). The seal was tested with valsalva and did not produce leak.
The patient was neurologically intact after the operation. Post-operatively the patient was well; she experienced a few headaches but still had no neurological deficit. According to the patient, sensation in the L2/3 distribution improved by approximately 70%. The patient was recovering well when suddenly, 48 hours post-operatively, the patient experienced four generalized tonic-clonic seizures, and was deeply post-ictal following the seizures. A diagnosis of tonic-clonic seizures secondary to low intracranial pressure was made.
All routine blood investigations as well as blood Amisulpride and Olanzapine levels carried out on all post-operative days were found to be within normal limits. A post-operative head/brain computed tomographic (CT) scan showed no infarct, haemorrhage or mass lesions. The patient was started on oral Phenytoin 3mg/kg daily and had no further episodes of seizures. She was successfully discharged 5 days post-operatively.
The patient was followed-up by a consultant neurologist monthly for 6 months. She never reported any problems during the duration of follow-up and was successfully discharged back to the community.
DISCUSSION
Dural tears during spinal surgery are not uncommon, with reported incidence rates of 0.3% to 17% (1, 2). Problems arising from this complication are rare, but devastating and require astute recognition of the early signs of neurological impairment. Here we are attempting to make an association between the CSF hypotension caused by an unintentional durotomy at lumbar surgery and the new onset of epilepsy which might have been propagated by the patients’ pre-operative anti-psychiatric medication.
The phenomenon of intracranial haemorrhage remote from a surgical site has been described in the literature, and several authors have attempted to explain the pathophysiology (1, 2). Although intracranial haemorrhage did not occur in this case, the same pathophysiology is thought to have contributed to provoke the new onset epilepsy. The so-called sag model postulates that haemorrhage results from altered cerebrospinal fluid hydrodynamics, causing caudal sagging of the cerebellum with stretching of cerebellar vermian veins (1).
Taking this pathophysiology into account, we admit that the dural breach was indeed very small. This was satisfactorily repaired intra-operatively, however, the CSF leak was substantial and the dura may have been weakened and prone to later leak. We hypothesize that this may have resulted in delayed intracranial hypotension, causing primary tonic-clonic seizures and not an intra-cranial bleed. Thus, we believe that the hypotensive insult coupled with an already lowered seizure threshold, due to the patient’s long term anti-psychiatric medical history, gave rise to these new onset tonic-clonic seizures. We are unaware of any cases of new onset epilepsy post-durotomy.
Although dural rupture during surgery and CSF hypovolemia are thought to be the main contributing factors to the above, we have great reservations about the types of chronic medications the patient was having. One may only postulate about the association between both Olanzapine and Amisulpride and their epileptogenic side effects. In the British National Formulary both drugs are classed as rarely causing epileptic side-effects. A case report published by Woolley and Smith (3) shows that atypical neuroleptics like Olanzapine and Amisulpride lower seizure threshold. Manufacturer's trials gave a seizure rate, similar to other antipsychotics, of 0.88% patients (product data sheet, Eli Lilly). In this article it is stated that the patient in question represents the strongest case to date implicating olanzapine alone in lowering seizure threshold, with objective EEG support. The manufactures data for both drugs issue warnings in their literature stating that both Amisulpride and Olanzapine can lower seizure threshold and therefore should be used with caution in patients previously diagnosed with epilepsy. However, they do not state that in cases where the seizure threshold is already lowered for example by CSF hypotension, new onset epilepsy might be more common (4).
In conclusion, new onset seizures following dural tears might appear in patients on anti-psychiatric medication. We strongly recommend that patients on potentially epileptogenic medication are either changed to other forms of anti-psychiatric non-epileptogenic medication or are closely monitored post-operatively in the event of this rare complication developing.



