-
PDF
- Split View
-
Views
-
Cite
Cite
T Buset, L Vaudoisey, N De Saint Aubain, R Javadian, X Vanden Eynden, Z Valyi, D Dequanter, Effective diagnosis and surgical management of primary signet ring cell carcinoma of the eyelid, Journal of Surgical Case Reports, Volume 2023, Issue 7, July 2023, rjad408, https://doi.org/10.1093/jscr/rjad408
Close - Share Icon Share
Abstract
Primary signet ring cell carcinoma of the eyelid is an aggressive and rare neoplasm. It generally develops from the eccrine sweat gland and diffuses to the dermis and subcutis of the eyelid or axillae. The lesion usually presents as a progressive, diffuse and painless swelling of the eyelid with or without erythema and is frequently misdiagnosed as a chalazion or a chronic blepharoconjunctivitis leading to delayed management. The histology typically shows a signet ring cell or histiocytoid morphology. The authors present a case of a 76-year-old woman with a diagnosis of a primary signet ring cell carcinoma of the eyelid with atypical presentations. With this report, we seek to increase clinician awareness toward this tumor and to highlight the need for systematic recommendations in order to improve the management of these patients.
INTRODUCTION
Primary signet ring cell carcinoma of the eyelid (PSCE) is a rare and aggressive neoplasm [1, 2]. In the literature, PSCE can also be named primary infiltrating signet ring carcinoma, histiocytoid variant of eccrine sweat gland carcinoma or adenocarcinoma of eccrine sweat glands [3]. This tumor develops from the eccrine sweat gland of the eyelids or less commonly the axillary region and typically diffuses into the dermis and subcutis [4, 5]. Elderly males are most frequently affected (82%) [4]. The periorbital lesion usually presents as a progressive, diffuse and painless swelling of the eyelid with or without erythema. In some cases, it may cause a closure of the eyelid leading to a ‘monocle-like’ appearance [6]. The tumor is frequently misdiagnosed as a chalazion or a chronic blepharoconjunctivitis leading to delayed management [1].
The rarity of this tumor often leads to delayed diagnosis and management. In this article, we report a patient with primary signet-ring cell/histiocytoid carcinoma of the eyelid and highlight the need to increase clinician awareness toward this pathology.
CASE REPORT
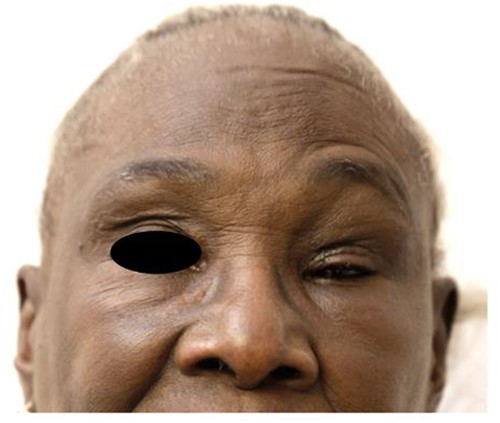
A 76-year-old woman presented to an ophthalmology consultation for a routine follow-up. She had a medical history of systemic lupus erythematosus treated with hydroxychloroquine, a ventriculoperitoneal shunt for hydrocephalus, chronic subdural hematoma, arterial hypertension and bilateral cataract which led to a decompensated esophoria. During the consultation, the patient reported a sensation of a mass pushing on her left eye with a feeling of eyelid closing and constant tearing on the same side (Fig. 1). The physical examination showed only a slight enophthalmos confirmed by a Hertel exophthalmometer showing a 1-mm difference between the two eyes. No other lesion was visible despite rigorous examination.
Three months later, an increased enophthalmos was noted. A magnetic resonance imaging (MRI) showed a thickening of the left upper and lower eyelids, up to the outer and inner canthus, infiltrating the glandular compartments and the lacrimal collectors without altering the intra or extraconic retro-septal fat. The infiltration was also observed in the superior, lateral and lower rectus muscles and the superior oblique muscle without any significant bone damage (Fig. 2). A biopsy of the left upper eyelid revealed infiltration of signet-ring cells and histiocyte-like cells. An extensive clinical workup, including whole-body positron emission tomography using fluorodeoxyglucose (FDG), did not identify any lesion in the left periocular region nor any extra-ocular FDG-avid lesions. A breast MRI was also performed to exclude a primitive breast carcinoma, while an oeso-gastro-duodenoscopy and colonoscopy did not show any sign of primary tumor or metastases.
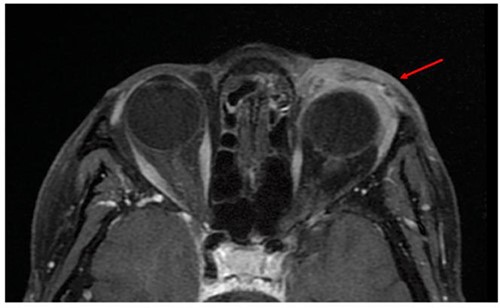
MRI showing a thickening of the left preorbital soft part (arrow), infiltrating the glandular compartments and lacrimal collectors with no alteration of intra or extraconic retro-septal fat.
The treatment consisted of a left orbital exenteration including the muscles, nerves and fatty tissues to beyond the periosteum of the orbit cavity and the upper and lower eyelid, associated with neck dissection for lymph node removal of zones Ib, IIa, b, III and IV (Fig. 3A, B, C, D, E). The reconstruction consisted of a free anterolateral thigh flap with microvascular anastomosis to the facial artery and to the thyrolinguofacial trunk was used to cover the defect.
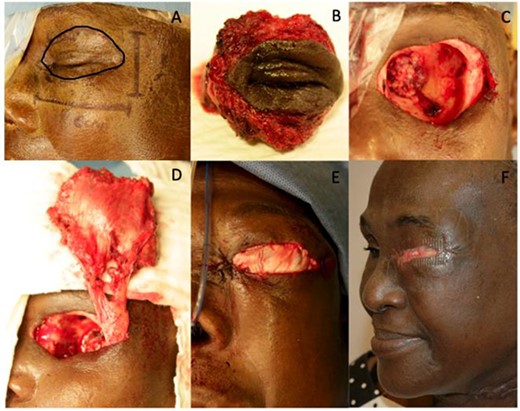
A: Delimitation of the cutaneous resection; B and C: left orbital exenteration including the muscles, nerves and fatty issues to the beyond to the periosteum of the orbit cavity and the upper and lower eyelid; D and E: reconstruction with a free anterolateral thigh flap used as an island flap; F: 3-month post-operative picture of the patient.
Post-operative microscopic examination revealed a widespread tumoral infiltration within the resected specimen (Fig. 4). The tumor extended across the lower and the upper eyelids, the periorbital adipose tissue and the muscle plane. No infiltration of the ocular structures such as the sclera was identified. Samples obtained after fixation and paraffin embedding showed abundant tumor cells characterized by a central vacuole and an eccentric and nucleolated nucleus and a characteristic signet-ring. The margins of the resected piece and of the lymph nodes were tumor-free without any residual malignant cells. The follow-up consisted of an MRI 3 months after surgery and a closed follow-up (Fig. 3F). No other adjuvant treatment was offered. Three years post-surgery, no recurrence has been observed clinically or radiologically with an MRI of the orbit performed 3 years after the surgical treatment.
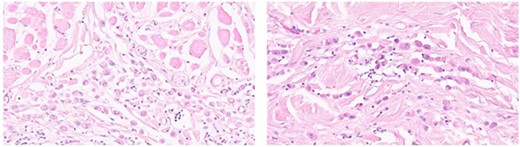
Histology of signet-ring cell/histiocytoid carcinoma of the eyelid in the subcutis and dermis; samples obtained after fixation and paraffin embedding showed numerous tumor cells with a central vacuole and an eccentric, nucleolated nucleus; those tumoral cells were identifiable by an abundant clear or eosinophilic cytoplasm and a characteristic signet-ring.
DISCUSSION
PSCE of the eyelid is the rarest of eccrine sweat gland carcinomas with only fewer than 50 cases reported in the English literature [2, 7]. It presents as an indolent low-to-intermediate grade malignant tumor of the eyelid [3].
We present here an atypical presentation of a PSCE of the Eyelid occurring in a woman [6, 8]. While most of these tumors present as a progressive and diffuse swelling of the eyelid that typically [3, 6] extends in a circumferential fashion to the orbit and ultimately leads to the closure of the eyelid, our patient first presented with isolated enophthalmos which led to a significantly delayed diagnosis until histological examination. Enophthalmos is rarely of a tumoral origin [6, 9, 10]. Orbital metastases, especially breast cancer, may induce a posterior displacement of the eyeball caused by an intra-conal cellular infiltrate, with the ability for contraction of the orbital content [10].
PSCE mimics metastasizing signet-ring cell adenocarcinoma, particularly tumors from the gastrointestinal tract, the breast and the urinary bladder and a complete assessment must be carried out to exclude such a metastatic lesion [5].
Considering the rarity of the disease and the limited number of reported cases, therapeutic guidelines are difficult to propose [2]. The treatment modalities for PSCE proposed by Tanboon et al. [8] based on the few cases reported in the literature include radical excision with wide margins and in case of extensive involvement of the ocular adnexa or orbital invasion, an orbital exenteration [6, 11]. A high incidence of local recurrence is expected in case of incomplete tumor excision so adjuvant radiotherapy with or without antiestrogen therapy (tamoxifen) or chemotherapy (5-fluorouracil) are recommended but lead to variable degrees of local control [3, 8, 12, 13]. In our report, we successfully followed these recommendations, confirming its efficacy after 3 years of follow-up.
In conclusion, we report an atypical presentation of signet-ring cell/histiocytoid carcinoma of the eyelid in a 76-year-old woman who initially presented with isolated enophthalmos. She was treated by left orbital exenteration without any adjuvant therapy. There was no evidence of recurrence or metastasis after a 3-year follow-up. With this report, we seek to increase clinician awareness toward this tumor, especially atypical presentations and to highlight the need for systematic recommendations in order to improve the management of these patients.
CONFLICT OF INTEREST STATEMENT
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
FUNDING
The authors received no financial support for the research.
AUTHORS’ CONTRIBUTIONS
BT: Manuscript writing.
VL: contribution to writing.
JR: Manuscript revision.
VZ: Manuscript revision.
DN: Manuscript revision.
DD: Manuscript revision, manuscript content approval.



